[edit]
SARS-CoV-2 Vaccine Development & Implementation; Scenarios, Options, Key Decisions
This paper has drawn on evidence available up to 25th September 2020. Further evidence on this topic is constantly published and DELVE will continue to develop this report as it becomes available. This independent overview of the science has been provided in good faith by subject experts. DELVE and the Royal Society accept no legal liability for decisions made based on this evidence.
Summary
The SARS-CoV-2 pandemic has led to a global effort to develop, test, manufacture and distribute effective vaccines at unprecedented speed. There are currently over 200 vaccine candidates in development and the results of initial large-scale trials are expected soon; however, to deliver a successful vaccination programme, many challenges remain. This report discusses the key issues involved in developing, evaluating, manufacturing and distributing a vaccine for COVID-19, the impact of those challenges and future strategies to mitigate their effects.
Citation
(2020), SARS-CoV-2 Vaccine Development & Implementation; Scenarios, Options, Key Decisions. DELVE Report No. 6. Published 01 October 2020. Available from https://rs-delve.github.io/reports/2020/10/01/covid19-vaccination-report.html [pdf].
Table of Contents
- SARS-CoV-2 vaccines
- Ensuring the success of a vaccine programme: vaccine efficacy
- Ensuring the success of a vaccination programme: vaccine availability
- Ensuring the success of a vaccination programme: vaccine acceptability
- Safety, tolerability, effectiveness and routes of administration may influence vaccine acceptability
- Clear communication is needed to build trust in vaccines, increase acceptability and thus effectiveness
- Barriers to vaccine uptake need to be minimised
- Priority groups will often require dedicated focus accounting for specific needs and concerns
- Requirements and consequences of vaccination programmes, possible scenarios
- Long-term lessons and preparedness
- Long-term effectiveness and safety of vaccines in different populations should be monitored
- A coordinated global vaccination programme and support for development of second-generation vaccines is needed
- Investment in vaccine R&D, global organisation and public perceptions of vaccination will aid pandemic preparedness, UK plc and support global health in the long term
Appendices
Key Points
-
A successful vaccination programme must consider the suitability of different vaccines. Key information that is needed to evaluate vaccines includes the ability to prevent disease in different groups, such as older people; the longevity of the immune response; the requirement for multiple doses and boosters; the ability to reduce infection and transmission of the virus; the tolerability and safety; the ability to be manufactured, distributed and administered at scale, affordability, and access and acceptability. Many of these properties will be unknown until well after the initial data on the first vaccine trials emerge.
-
Long term studies will be needed to establish vaccine effectiveness and longevity of protection. Few vaccines give lifelong protection following a single dose. A partially protective vaccine may not be effective in priority groups, may allow onwards transmission, or could require higher vaccination rates to achieve the same levels of protection in a population. A vaccine of low efficacy may not achieve herd immunity. Rare adverse events or limited effectiveness in the field may only come to light when very large numbers of people are vaccinated. Multiple doses may be needed to stimulate an effective level of immunity and if a candidate yields short-lived immunity, boosters may be required, with implications for manufacturing capacity, distribution and for generation of immunity in the wider population.
-
Further research is needed to understand the immune response to SARS-CoV-2 and the levels of immunity required for protection, and if and when immunity wanes. We do not yet know which immune responses can protect against infection and can only determine whether a vaccine protects against disease by carrying out large scale trials. A better understanding of which immune responses are protective, using data from animal models, clinical trials and potentially human challenge studies will allow us to determine the correlates of protection and measure protection at an individual and population level. Standardisation of vaccine trials is needed to allow comparison and evaluation of different candidates.
-
Manufacturing will need to be scaled to meet the enormous demand of a global immunisation programme and vaccine availability is likely to be limited initially, requiring prioritisation of recipients. The scale of manufacture required will depend on knowing the amount of active ingredient needed per dose, the number of doses needed, the production process needed and how long it will take to manufacture. Candidate vaccines using new technology are as yet unproven in their ability to be produced at scale but have the potential to be vastly more efficient in production than well-established platforms. For the overall vaccine manufacturing process, the bottlenecks could be the fill-to-finish process whereby the drug substance is filled into vials or other containers and the so-called drug product is obtained. Although some facilities can be repurposed, this is not the case for all stages in manufacture.
-
The vaccine manufacturing-distribution-administration chain represents a complex system with multiple parts and multiple objectives which are sometimes competing. Production may be limited by supply chains of materials and delivery systems. The requirements for storage and transportation may limit distribution and access globally. Efforts might be required to improve thermostability of vaccines and minimise the requirement for low temperatures for distribution. The most important bottleneck here appears to be the final administration step. Administration of a vaccine will require a large number of appropriately trained health workers with access to - and relationships with - different communities.
-
Unequal access and vaccine availability risks exacerbating health inequalities. Ethnic minority groups have been disproportionately impacted by the pandemic and overcoming barriers to vaccination will require culturally sensitive collaboration. Criteria for vaccine prioritisation should be defined and made explicit. There should be public dialogue and engagement to manage expectations and understanding of vaccine effectiveness, safety, side effects, availability and access.
-
The diverse reasons for vaccine hesitancy will need to be addressed to engender public trust, with clear messaging targeted to different groups. Acceptability will be determined by factors such as efficacy, doses required, side-effects, and perceived risks. There are a number of reasons for vaccine hesitancy and a range of strategies are needed, such as ‘convert communicators’, where those with previously strongly held opinions explain why they changed their mind. Other barriers to vaccine uptake such as financial disincentives should be removed.
Vaccine strategies will need to be planned and revised on the basis of an integrated understanding of the emerging data on immunology, economics, manufacturing and behavioural issues, which will govern a successful vaccination programme.
-
Global collaboration is needed to ensure that vaccines will be affordable and available equitably, ensuring the greatest health outcomes. International collaboration reduces the risks of investment and helps to secure global supplies and affordability.
-
Global coordination and investment will be needed in the longer term to provide preparedness for future pandemics. The development of second-generation vaccines should be incentivised. Global coordination will be needed to protect all nations against outbreaks. Strategic vision and investment in scientific innovation and understanding of infectious disease, vaccine design, testing and manufacture as well as public expectations of vaccination will provide long-term solutions and preparedness.
1. SARS-CoV-2 vaccines
The SARS-CoV-2 pandemic has led to a global effort to develop, test, manufacture and distribute effective vaccines at unprecedented speed. There are currently over 200 vaccine candidates in development. A successful vaccination programme will depend on understanding the properties and effectiveness of different vaccine candidates, their requirements for manufacture, distribution and administration, and public acceptability.
What constitutes an effective vaccine?
How do vaccines work?
The immune response that follows infection can provide a long-lasting immune ‘memory’ that protects against re-infection and disease. In the same way, vaccines protect by mimicking a natural infection to stimulate immune memory, but without causing disease. Most currently licensed vaccines stimulate production of antibodies that bind specifically to the virus eliminating the infection. Vaccines may also induce memory T cells. T cells enhance the antibody response as well as directly destroying virus-infected cells. While these are often protective, antibodies and T cells can cause unwanted harmful effects (i.e. immunopathology). Most vaccines under development for SARS-CoV-2 aim to stimulate an effective immune response to one component of the virus, the outer viral spike or S protein, whilst minimising the risks of adverse effects.
What makes an ideal vaccine?
An ideal vaccine is one that is safe and stimulates immune responses that reduce both the risk or the severity of disease and the chance of transmission of the infection. It should also confer long-term protection so people do not need to be frequently re-vaccinated. Few vaccines meet all these ideals.
Typically only a proportion of those vaccinated mount a sufficiently strong immune response to protect against disease (this is the vaccine efficacy), and particular groups such as older people often respond poorly to vaccines due to aging of the immune system. Vaccines typically also reduce transmission of the virus from those who have been vaccinated to others, and so protect those who are unvaccinated or respond poorly to immunisation, however a vaccine that reduces disease but not infection can theoretically still allow transmission to occur.
For example, influenza vaccines are usually only partially effective (particularly in the high-risk groups targeted such as older people) and changes to the circulating virus renders the immunity useless after a time, so annual re-vaccination is required. However, even partial protection can have important benefits, with for example the FluEnz nasal spray vaccine not only reducing disease in children but also reducing spread of disease to their older relatives.
What immune responses can protect against COVID-19?
We do not yet know which immune responses, if any, protect against SARS-CoV-2 infection. Antibodies and T cells can be detected in the majority of those who have recovered from SARS-CoV-2 infection, but it is not known whether infection leads to protection against reinfection or severe disease nor how long any immunity lasts. As such, we don’t know which types of immune response should be stimulated by a vaccine to protect against infection.
The role of antibodies
Evidence from natural infection with seasonal “common cold” coronaviruses suggests that immune responses generated after infection are associated with protection against re-infection. However, this response wanes and after a year re-infection may occur in about two-thirds of previously infected people, although most have few if any symptoms.1 Antibodies typically appear a few weeks after infection but wane within 2-3 years. Similar studies following SARS-CoV-2 infection are in progress. Currently, the only SARS-CoV-2 data are from non-human primates, in which the presence of antibodies that bind and block the virus correlates with protection.2 3 Neutralising antibodies can in principle act to prevent viral entry and replication in cells, thus preventing infection. Neutralising antibodies that bind to the outer spike (S) protein of the SARS-CoV-2 virus have been identified in most people who have recovered from infection, 4 5 6 7 8 but whether these are protective remains to be confirmed.
The role of T cells
SARS-CoV-2-specific T cells are detectable in convalescing patients following COVID-19,9 10 11 12 13 but their role in protection is not known. Studies have reported that virus-specific T cells are detectable even in those who do not have detectable levels of antibody, and in those who experienced mild or asymptomatic infection.13 14 Thus T cell responses may prove to be a more reliable test of prior exposure to SARS-CoV-2 than serological tests for antibodies, and a better test for population surveys of previous infection. However, the longevity of T cell responses is not known, and tests for the presence of T-cells are technically more demanding than those for antibodies. T cells produced following SARS-CoV (SARS) infection were still detectable after more than 11 years, whereas the antibody response waned over 2-3 years.15 16 17 Most studies of T cell memory to SARS-CoV-2 have been able to measure responses at least a month after symptom onset.
Generally, immunity is very specific for a particular infection, such that antibodies and T cells produced during SARS-CoV-2 infection will only recognise that virus. However, different coronaviruses may be similar enough to each other that T cells against coronaviruses are cross-reactive. Several groups have reported the presence of T cells in individuals with no evidence of SARS-CoV-2 infection, which nevertheless recognise SARS-CoV-2. These T cells may be developed in response to circulating common cold strains of coronavirus, 9 10 17 18 although not all reports agree. 12 Cross-reactive T cells may contribute to protection against COVID-19, potentially reducing severity of infection, and influencing responses to vaccination. 10 If so, then vaccines that stimulate T cells are likely to confer more efficient protection than that given by antibodies alone.
Immune enhancement of disease
While antibodies and T cells are often helpful, they can also be destructive and enhance inflammation if present in the wrong proportions or mis-targeted, or if they enhance entry of the virus into cells. Historically, this has occurred with some vaccines (which commonly focus on inducing high levels of a single type of immune response), leading to vaccine-enhanced disease. There is a risk that this could occur following vaccination against SARS-CoV-2.19 20 21 Antibody dependent enhancement (ADE) occurred following vaccination against a feline coronavirus20 22 and the potential for antibody enhanced uptake of virus can be demonstrated in the laboratory for the related MERS and SARS-CoV-1 viruses.23 24 25 Animal models of SARS-CoV-2 infection for vaccine development may prove useful for assessing safety in this context 26 but there is currently no reliable predictive measurement of immune enhanced disease, whether in all recipients or in individuals.21 Although this remains a theoretical risk, all clinical vaccine trials should therefore include long-term follow-up of vaccinated individuals at sufficient scale to assess for unexpectedly severe disease on subsequent natural SARS-CoV-2 infection that might be due to immune enhancement.
What is the current situation with vaccines in clinical development?
Over 200 SARS-CoV-2 vaccine candidates are currently in development 27 28 29 30(Appendix 2). Some candidates that are in the later stages of clinical trials (e.g. the Oxford/Astrazeneca ChAdOx1) are based on “viral vectors”, where part of the SARS-CoV-2 genetic code is inserted into another harmless virus. 31 32 33 34 When the harmless virus enters a cell, it produces the SARS-CoV-2 S protein which stimulates the immune system to produce antibodies and memory cells against this viral protein. An alternative design is where the viral genetic code is produced as an RNA vaccine (e.g. Moderna), which also leads to the production of viral protein when it enters a cell. 35 Other candidates include protein subunit-based vaccines, where viral protein is produced in culture, and inactivated virus, where the whole virus is grown in culture, before being inactivated. Some vaccines will be formulated with adjuvants, which promote inflammation that enhances antibody production. Some of the current vaccines in development, such as inactivated virus formulations, are based on well established technologies with a track record of widespread use, whereas others, such as RNA vaccines, have not previously been used in a licenced vaccine. For the purposes of speed, almost all vaccines under development will be delivered intramuscularly as this is the simplest and best understood mode of delivery. However, since intramuscular injections do not specifically stimulate antibodies or T cells in the nose or lung, they may not be the most efficient at preventing disease or transmission in the airway.
Clinical development of these early candidates has been accelerated to an unprecedented level, with the Oxford, Moderna and Sinovac vaccines among those that have started large-scale field trials internationally. However, the history of vaccine development is littered with candidates that have failed at this late stage, due for example to poor immunogenicity, and there is no guarantee that these vaccines will be effective. If vaccines were deployed outside clinical trials before safety and efficacy have been fully established and prove to be ineffective or cause rare but severe side effects during the larger-scale roll-out, they could cause substantial harm and damage public confidence in other vaccines. Strict regulation of clinical trials and robust licensing rules must therefore be maintained in spite of the urgency and requirement for speedy implementation.
As data from vaccine trials emerge, vaccine candidates will need to be evaluated for their suitability for use in different populations. The success of a vaccine programme will depend on vaccine efficacy, availability and uptake.
2. Ensuring the success of a vaccine programme: vaccine efficacy
-
Vaccines are unlikely to yield 100% protection in all recipients and may vary in their ability to produce immune responses and memory to SARS-CoV-2
-
As a result, vaccines might have differing abilities to prevent disease and transmission in different groups and the longevity of protection
-
Standardisation of clinical trials and immunological laboratory tests is required to evaluate and compare different vaccine candidates
-
Correlates of protection need to be established to enable rapid monitoring of immunity in individuals and the wider population
-
Partial protection following vaccination may require multiple doses and boosters to achieve immunity at an individual level and high levels of vaccine coverage in a population to achieve immunity
-
Animal models and human challenge studies may increase our understanding of immunity to SARS-CoV-2 and expedite vaccine development
-
More basic research is needed to understand the nature of protective immune responses to SARS-CoV-2 infection
Testing and evaluation of vaccine candidates
Different vaccine candidates have different properties
Different vaccines will generate distinctive immune responses, and therefore have different abilities to prevent infection, transmission and disease. Immunity generated may be mainly antibody-mediated or a more balanced antibody and T cell response.36 A variety of T cell types can be produced, with different abilities to protect against infection and form memory cells. Memory may be short or long-lived. Different vaccines may require single or multiple doses to induce a good memory response and will differ in the immediate unwanted side effects (reactogenicity) that will influence vaccine uptake and acceptability.37 Vaccines may work less well in certain groups, particularly in older people who often respond poorly to vaccination and are particularly vulnerable to SARS-CoV-2.
While preventing lung disease is a key goal of a vaccine, stopping transmission may not be possible if infection and viral shedding still takes place. This may depend on the route of immunisation and the subsequent location of generated immunity. Systemic vaccination via for example injection into a muscle, may not induce good local immune responses in the airways, so may not prevent upper respiratory tract infection, viral shedding or transmission even if it protects the lung. This phenomenon has been seen in non-human primates studies.3 The majority of vaccines currently under development administer the vaccine by the intramuscular route. Phase III clinical trials currently underway use a reduction in COVID-19 disease in vaccine recipients as their primary endpoint, and information on the ability of the vaccine to prevent onward transmission will not be available. Although most vaccines do prevent both disease and onward transmission, transmission remains a possibility that would need to be studied in community trials where the incidence of infection in unvaccinated recipients is determined.
The efficacy of a vaccine, that is its ability to protect an individual, under ideal circumstances in the context of a clinical trial, should be distinguished from effectiveness of a vaccine which is determined as the sum of reduction in clinical events in the real world and which is influenced by both vaccine efficacy and many other factors.
Identifying correlates of protection will aid measurement of vaccine efficacy
Vaccine trials will determine the efficacy of protection against symptomatic infection within a relatively short time. For many vaccines, having high levels of antibodies and/or T cells is associated with efficacy. These immune markers may then act as correlates of protection so that their measurement can be used as a surrogate to predict vaccine efficacy.38 39
Once correlates of protection are identified they might be used in vaccine trials and allow researchers to estimate vaccine efficacy before larger scale or more complex trials such as population-level field studies (which take time and large numbers of volunteers) or human infection challenge studies with deliberate infection of volunteers (which tend to be small scale and have accompanying risks with ethical implications that need careful thought (Appendix 1). If the correlates are well understood, they might be used to rapidly assess whether an individual responds to a vaccine and is likely to be protected. Appropriate correlates of protection for SARS-CoV-2 are not yet known. Correlates will probably differ depending on the desired outcome measure, such as protection against infection itself, prevention of symptomatic infection or severe disease, or transmission.38 Protection invoked by a vaccine may rely on different components of the immune system to those that develop following natural infection.
In cases where antibody protects against a virus infection, we need to measure the amount of antibody produced following vaccination (the antibody titre) and know whether this is above a protective threshold. Measurement of antibodies in the blood, the most commonly used correlate of protection, is relatively simple to perform in diagnostic laboratories, and can be standardised across different laboratories by use of reference samples. We do not yet know if there is an antibody level that represents protection against SARS-CoV-2 infection. Further complexity is added because as well as the quantity of antibodies, the properties of the antibodies will determine how well they protect. Neutralising antibodies which block the ability of the virus to infect cells may be the best correlate of protection, but neutralisation assays are technically difficult and are not used for routine diagnostic tests. Many commercial tests detect antibodies to the nucleoprotein (N) of the virus to which there is a strong antibody response. While this helps to maximise sensitivity of the test, N protein is found on the inside of the virus particle, so these antibodies may not prevent infection nor act as a good correlate of protection.
Whilst antibodies are an easily accessible and measurable component of immunity, a balanced and efficient immune response includes the formation of long-lived memory T cells to provide optimal protection against re-infection. However, T cell measurements are difficult to carry out and techniques used differ in different laboratories. Nevertheless, work is ongoing to develop and partially standardise these methods in both academic and commercial labs. The U.S. Food and Drug Administration (FDA) recommends that studies of the immune response to vaccine candidates should include both antibody responses, including neutralisation assays, and assessment of the T cell responses.40
Standardisation of Clinical Trials
SARS-CoV-2 vaccine trials, in prioritising speed due to the critical health need, may generate data that are difficult to interpret. Different trials have employed different methods both in the design of the study and in the laboratory measurements used. This will make comparing the relative merits of different vaccine candidates difficult. Standardisation of study design and agreeing on core end points and their hierarchical ordering in vaccine trials will allow comparison of different vaccine candidates and aid vaccine development. One difficulty in establishing correlates of protection is that different tests may be performed by different laboratories using different definitions of immunity. Standardisation of immunological assays as well as clinical endpoints would allow comparison of data across trials.41 International availability of and requirements to use standard reagents will ensure consistency across different studies.
Funders such as The Coalition for Epidemic Preparedness Innovations (CEPI) have made efforts to standardise the studies they support but comparability of data will need to be a priority for both funders and policymakers. This is particularly important when considering the differences between studies conducted in different countries.
Furthermore, while there is good evidence that some minority ethnic groups have experienced worse COVID-19 health outcomes than their white counterparts, it remains the case that volunteers from ethnic minorities are routinely under-represented in trials even when these groups are specifically targeted with advertising and public engagement.42 Trial populations should be reported and reflect the ethnicity of the groups most affected by the pandemic. Since the pandemic has amplified inequalities associated with ethnicity and health it is essential to understand why volunteer participation in some minority groups is low and how to increase vaccine acceptance in them.
Limitations of Clinical Trials
Outside of pandemics, clinical vaccine development is a slow and incremental process to ensure safety and reduce the risk of cumulative investment in products which fail due to ineffectiveness or side effects. Clinical trials are thus typically divided into phases I, II and III, which take place sequentially, investigating safety in the early phases and efficacy in large scale trials later with increasing numbers of volunteers required. This has been accelerated in the testing of SARS-CoV2 vaccines. Efficacy can only be shown when there is sufficient circulation of the infection to demonstrate a reduction in cases in vaccinated people. Studies in Brazil, South Africa and the USA are likely to be the only ones in which this may be currently possible for SARS-CoV-2, although targeting high-incidence groups such as healthcare workers may have a role. There are risks that study quality might suffer if clinical trials are accelerated to catch pandemic waves.43 There are also implications for the ethics of vaccine studies in low and middle income countries (LMIC), public trust and vaccine acceptance, as highlighted by recent demonstrations in South Africa against some vaccine studies, which some believe to be exploiting local populations.44
The FDA has stipulated a requirement of 50% efficacy for licensure.40 Current trials primarily measure efficacy as a reduction in symptomatic infection, rather than infection per se or severe disease, furthermore different trials use different definitions of symptomatic infection. The first vaccine trials will not tell us how long immunity lasts and the need for booster doses. They will not reveal whether onwards transmission occurs if for example, symptoms are reduced but mild or asymptomatic infection still occurs. Long term and rare side effects may not be detected and so long term phase IV safety monitoring will be essential once vaccines are licenced for clinical use.
Benefits and Limitations of Animal Models
Animals, including non-human primates (NHP), have been used to determine whether protective immunity is generated following SARS-CoV-2 infection, to test vaccines and determine protective mechanisms. Safety testing of vaccines in animal models can help to predict potential harmful effects including vaccine enhanced disease upon infection. Non-human primates can be infected with SARS-CoV-2 as they possess a similar ACE2 receptor (which the virus uses to infect cells) to humans2 45 46 and SARS-CoV-2 challenged or vaccinated rhesus macaques demonstrated protection against reinfection.2 3 47 Small animals can also be infected, including transgenic mice which have been engineered to express the human ACE2 receptor.48 49 50 51 52 53 The Syrian golden hamster in particular has emerged as a suitable animal model for SARS-CoV-2 and has been used to demonstrate the protective effect of antibodies.54 However, data from animal experiments must be interpreted with caution. Rechallenge studies have so far been undertaken only a short time after vaccination or primary infection, so the longevity of protection is not known, furthermore variation in models employed reduces our ability to compare different vaccines.33 55 Animal immune systems differ fundamentally from the human immune system in certain respects we understand and possibly ways we do not understand yet, experimental animals are often housed under unusually clean conditions and lack experience of infections and other diseases, and the doses of virus used in animal experiments tend to be much higher than those encountered in natural human infection.45 49 51 56 NHPs are currently viewed as the most useful model but are very expensive so numbers used are very small. NHPs are also outbred so results can be highly variable and most animal models (including NHPs) do not show much disease or pathology with SARS-CoV-2.
Can human infection challenge studies accelerate vaccine development?
To address gaps in understanding of protective immunity and to develop a strategy for selecting or rejecting vaccine candidates, human infection challenge with SARS-CoV-2 is being considered57 (Appendix 1). Human infection challenges with influenza and other respiratory viruses have been conducted safely for many decades and have provided critical knowledge for the development of vaccines. By deliberately inoculating volunteers with a well-characterised virus, a consistent and guaranteed high infection rate is achieved so fewer participants are required to show evidence of protective efficacy. Vaccine testing therefore avoids relying on exposure of individuals to natural infection in the community, which may be limited or unpredictably variable. Using a human challenge system, candidate vaccines can be quickly assessed for the immunity they elicit and whether that affects the infection rate. In the case of SARS-CoV-2, the novelty of the virus and uncertainties about effective treatment or long-term complications require careful consideration to balance the risks to individual volunteers and benefit to society in accelerating the development of effective vaccines, especially when field trials using community exposure are still possible albeit only in some places.58 59 60 The WHO has published an ethical framework for SARS-CoV-2 challenge studies and a number of groups are considering strategies to mitigate risk. Specifically, COVID-19 is now known to cause mild or asymptomatic disease in the vast majority of young adults, so restricting the age range of enrolled volunteers and limiting disease with antivirals may render the system safer. This is clearly a limitation in that vaccines cannot be tested in groups such as the older people in whom the risks of challenge are higher. Furthermore, challenge studies do not tell us about the effectiveness of a vaccine programme in the real world. Key steps to developing this model will be to generate a stock of SARS-CoV-2 that is suitable for administration to volunteers; expert consensus on how such studies should be run safely; and identification of the facilities and resources to conduct the studies while minimising risk to study participants and people in the surrounding community to an acceptable level.
Partially effective vaccines
The ideal vaccine would generate life-long immunity to infection following a single dose. In reality, this level of protection is frequently not achieved and SARS-CoV-2 vaccines in development are unlikely to result in complete protection against infection in all recipients.
Partial immunity in a population may result from differences in the way individuals respond to the vaccine, with only a proportion of those immunised producing a strong enough immune response to be protected. Vaccine efficacy is typically measured as the proportion of those vaccinated who are protected from symptomatic infection. For example, inactivated influenza vaccines have an average efficacy in preventing confirmed influenza infection of around 59% of individuals.61 Differences in the response of individuals to a vaccine may in part be explained because certain groups, such as children or older people, often respond poorly to vaccines.
Partial immunity in an individual may result because the response generated by a vaccine does not completely protect recipients against infection, but for example, reduces the severity of disease. Viral replication might be reduced but may potentially allow transmission to occur. For example, the recent trials of the ChAdOx1 nCoV-19 vaccine in primates, resulted in a reduction in clinical severity and amount of virus in the lungs of vaccinated animals, but did not reduce viral shedding from the nose.33
Partial immunity might result because over time protective immune memory responses wane. Re-exposure to the pathogen or a booster vaccine can reactivate immune memory and restore levels of protective immunity. Partial immunity may also theoretically contribute to immune enhancement on subsequent infection due to imbalances in the different arms of immunity.
The WHO gives a Target Product Profile for a SARS-CoV-2 vaccine as inducing a minimum of 6 months but preferably at least a year of protection, with efficacy in at least 50% of the population (preferably 70%) including in older people.62
We show in Figure 1 how these concepts are related to population-level immune responses to SARS-CoV-2 due to natural infection or vaccination.
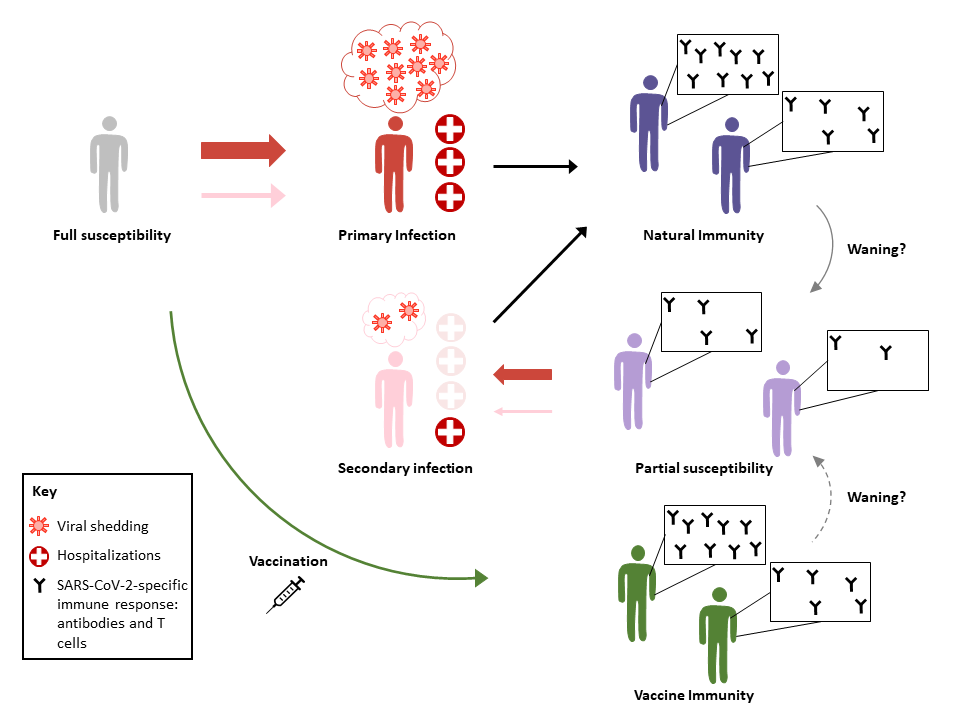
Figure 1: Population-level immune responses to SARS-CoV-2 infection. Primary infection gives rise to different degrees of immunity in different individuals (dark blue population, top right). Over time, this natural immunity may wane, making some individuals susceptible to secondary infection. People with primary infection typically experience more severe disease and shed more virus than those with a secondary infection, and so are more infectious (larger red arrows than pink arrows). Fewer people with secondary infection are likely to need hospitalization than those with primary infections, although there is a theoretical risk of greater severity in secondary infections due to phenomena such as antibody-dependent enhancement. An effective vaccine would provide immunity to fully susceptible individuals without requiring infection, although this immunity may also wane, possibly at a rate different from natural immunity.
Partial immunity means higher vaccination rates are required
Intuitively, if the proportion in the population vaccinated with an effective vaccine is sufficiently high, then immunity generated by a fully transmission-blocking vaccine could control or eliminate the infection: this is called herd immunity. However, herd immunity becomes harder to achieve when vaccine-induced or natural immunity is partial and/or short-lived, allowing secondary infections to occur, or when logistical or other constraints limit vaccine deployment and coverage. The authors in63 employed simple epidemiological models to explore the impact of a partially transmission-blocking vaccine on the timing and number of future COVID-19 infections. The analysis in63 assumes that vaccine immunity has a finite duration and reduces the vaccinated individual’s susceptibility to natural infection to a level below that of an unvaccinated person. Although successful vaccines may operate on the basis of the generation of a memory T cell or antibody response against the pathogen (as previously discussed in the immunology section), these details are not explicitly considered in 63, and instead are accounted for more generally through the parameters describing the effectiveness of the vaccine-induced immune response.
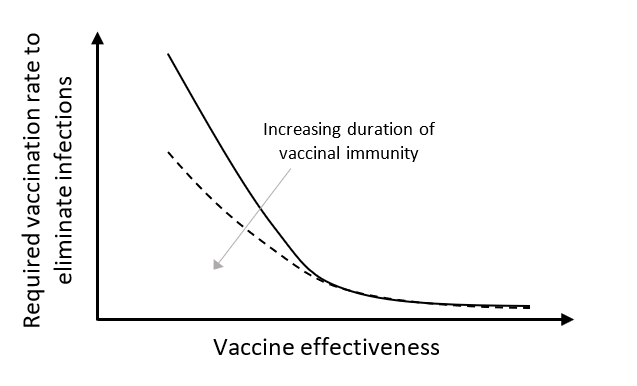
Figure 2: Schematic of qualitative vaccination rate required to eliminate infections as a function of the effectiveness and duration of vaccinal immunity adapted from.63
The results in63 suggest that both the effectiveness of a vaccine and the duration of the immunity it confers affect the vaccination coverage required to achieve a disease-free state at equilibrium (see Figure 2). With a fully transmission-blocking vaccine, relatively low vaccination rates are required to achieve zero infections at steady state. However, as immunity becomes more imperfect, increasingly high vaccination rates are required to eliminate infections particularly when the duration of vaccine immunity is short. This illustrates that reductions in infection achievable through vaccination are inherently related to the efficacy of the vaccine and the nature of the adaptive immune response, yet even an imperfect vaccine could have important impacts on SARS-CoV-2 infection dynamics and control.
Several practical aspects related to vaccine deployment bear mentioning in the context of the discussion of this work. For the most part,63 considers a uniform, well-mixed population, and the authors show that their results are qualitatively robust to considerations of heterogeneity in the transmission of and susceptibility to SARS-CoV-2 between individuals. However, the existence of these heterogeneities will necessitate a careful, equitable rollout and distribution of a vaccine when it becomes available, particularly if it is only partially protective and its initial availability is limited. Specifically, in order to reduce strain on healthcare systems, individuals at higher risk of acquiring severe infections (i.e. older people and those with comorbidities), or those with higher re-transmission potential might need to be prioritised.
What might influence the efficacy of SARS-CoV-2 vaccines?
The response to vaccination differs widely between individuals for reasons not completely understood. However, for SARS-CoV-2, older adults will be a particularly problematic group as they are both most susceptible to severe disease and less likely to mount an effective immune response following vaccination. This is likely due to ageing of the immune system. Potentially, emergence of new strains of virus might also limit efficacy of a vaccine. To enhance vaccine-induced immunity, strategies include repeat vaccination, vaccinating with higher doses, administering boosters and adding vaccine components that enhance immunogenicity by engaging other arms of the immune system (adjuvants). Different vaccines will stimulate different components of the immune response to differing degrees; some will induce higher levels of neutralising antibodies and others will induce a stronger T cell memory. Mucosally delivered vaccines may afford better protection at mucosal sites such as the respiratory tract.
Re-vaccination may be required as immunity wanes. The requirement for boosting will influence the choice of vaccine platform as not all vaccines will be suitable for repeated vaccination if immunity to the vaccine itself is acquired. This may occur particularly with viral vectored vaccines, where the immune response generated to the viral vector itself would remove the vector before it could sufficiently restimulate the immune system. A prime-boost strategy may therefore require a combination of different vaccines. The need for boosting has implications for the cost and access to a vaccine, potentially increasing the number of doses that need to be produced, requiring long-term increases in manufacturing capabilities and adding complexity to a vaccination programme, including acceptance. Prime-boost strategies must be specifically tested in clinical trials of appropriate groups.
Further research is required to determine how the immune response can protect against SARS-CoV-2
Ultimately, the ability to properly plan for the level of vaccination required and who to prioritise will depend on an improved understanding of the nature and duration of vaccine immunity, disease susceptibility and transmission.64 65 66 To interpret the results of different trials and to aid the design of future trials, further research is needed to understand which immune responses protect against infection and disease, and should be the goal of any vaccine candidate.41 How and which antibody responses and the threshold amount of antibody needed to protect against SARS-CoV-2 infection is not known. Most vaccines under development aim to elicit antibody responses to the S protein, but the importance of immunological recognition of other components of the virus is far less well understood and vaccines that include more than one component of the virus may prove to be more effective. In addition to neutralisation, different types of antibodies (isotypes) vary in their ability to direct other components of the immune response towards the virus or virally infected cells. However, the relative importance of different antibody isotypes to the outcome of SARS-CoV-2 has yet to be established.
Additionally, the location of antibodies and T cells may be critically important. It is likely that local immunity in the nose and lung will be more effective in preventing viral shedding and pneumonia. While antibodies and cellular responses are most frequently measured in blood due to ease of access, those found in the airways can be a better correlate of protection for respiratory infection than serum antibodies. For example, IgA, an antibody which is known to be produced following SARS-CoV-2 infection, may act as a first barrier to infection.67 These local immune responses are less well understood and therefore research in this area needs priority.
Further research is also needed to understand the timing of the T cell response, its longevity, what factors determine the development of good T cell memory and whether it is a good correlate of protection. If we can determine what parts of the virus are recognised by T cells these may be good candidates for inclusion in a vaccine. Furthermore, there are different types of T cells with different functions and the role of these subsets will need to be better understood so that the optimal T cells responses can be tested for and vaccines designed to promote these responses. T cells in the airway have special features that may enhance protection but are not stimulated by intramuscular vaccines, and mucosal vaccines, such as those delivered intranasally, might be particularly effective at stimulating production of these T cells. Investigating these features and standardising assays should overcome many issues resulting in conflicting data on T cell responses from different studies.
3. Ensuring the success of a vaccination programme: vaccine availability
-
Financial investment and advanced purchasing agreements have incentivised rapid development and production of SARS-CoV-2 vaccines and an increase in global capacity for vaccine manufacture
-
International collaboration in development of multiple vaccine candidates reduces the risk to individual countries and companies, and increases availability and affordability
-
Expansion of global vaccine manufacturing capacity represents a major challenge
-
Not all vaccines under development have a proven ability to be produced at scale
-
Supply chains for manufacture and distribution may limit availability
-
Administration of vaccines is a significant bottleneck and will require trained personnel working within communities
-
Unequal access to a vaccine risks exacerbating national and global health inequalities and might thwart efforts to control SARS-CoV-2 for all countries
Financial incentives for vaccine development
The COVID pandemic has caused enormous global economic damage. The International Monetary Fund (IMF) estimates that the cumulative output loss over 2020-21 could be USD 9 trillion, with the global economy projected to contract by 3% in 2020.68 In addition to the health impact, the macroeconomic impact of an effective SARS-CoV-2 vaccine has convinced governments, non-governmental organisations (NGOs) and industry to make unprecedented levels of investment to accelerate vaccine development and manufacture.
The typical economic model of development of any new pharmaceutical or vaccine is driven by identification of patient and market demand, large-scale high-risk R&D investment, patents that preserve market monopoly and prices set by willingness to pay and investment needs for future development. Historically, development of new vaccines is seen as high risk and has typically taken around 10 years at a cost estimated as between USD 500 million to USD 1-2bn, with a likelihood of entering the market of only 6-7%.69 70 71
Both ‘push’ and ‘pull’ incentives can be used to finance vaccine development and both have been used to accelerate the development of SARS-CoV-2 vaccines.72 73 74 ‘Push’ funding finances investment in basic research and development of both the vaccine and manufacturing capacity without the need for a specific goal to be achieved, thereby reducing the cost for the developer. ‘Pull’ funding has been used to accelerate the development, availability and uptake of vaccines and other medical products, by guaranteeing reward for successful development.72 74 75 An example of ‘pull’ funding are Advanced Market Commitments (AMCs), purchase agreements that can be used to guarantee price and quantity of vaccines purchased before the results of clinical trials are known and in advance of licencing.74 76 AMC have been used, most notably, by the global vaccine alliance Gavi, a public-private partnership, to secure supply of vaccines for preventing pneumococcal disease in low income countries.76 77 A purchase guarantee at a fixed price incentivises and de-risks vaccine development and investment in manufacturing capacity for the provider, and secures affordable vaccine supply for the purchaser,74 78 although AMC have been criticised for the relatively high price paid.79 The concerns about high prices may be ameliorated if joint negotiations are carried out by multiple countries. For SARS-CoV-2 vaccines such advanced investment in developing vaccines and manufacturing capacity before a vaccine is licenced will ensure rapid availability of vaccines once successful candidates are identified. In addition to securing vaccine development, supply chains for adjuvants and bioreactors need to be strengthened in parallel to avoid delays in and failure of vaccination drives.
Individual governments have acted to secure vaccine supplies. To date, the UK government is reported to have made forward purchasing deals to secure over 300 million vaccine doses, potentially enough for almost 5 doses per person,80 with the USA, European Union and Japan also securing hundreds of millions of doses81 (Table 1). The UK government has invested in vaccine manufacturing facilities to increase capacity, for example, in partnership with biotech company Valneva in Livingston, West Lothian, as well as supporting the fast track construction of the UK Vaccine Manufacturing and Innovation Centre (VMIC).82 83 Furthermore, the government has secured other necessary supplies for example, ordering 65 million injection devices for autumn 2020.84 The US government has invested in the development of vaccine candidates under Operation Warp Speed.85
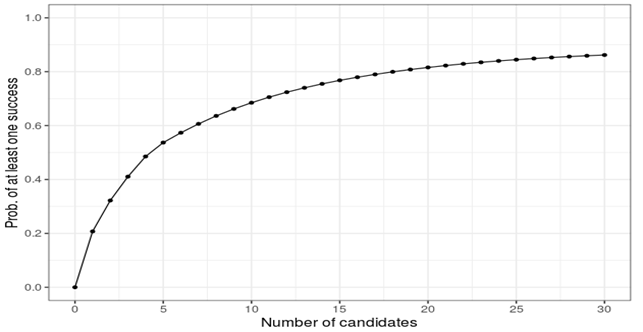
Figure 3: Probability of success as a function of number of candidates. Source: https://www.AcceleratingHT.org/.
It is advantageous for countries to unite in their negotiations with multiple firms for development and manufacturing of vaccines; this will ensure a higher probability of success, with more vaccination at a lower overall cost.86 The model illustrated in Fig 3 suggests that it would be optimal to invest in 20 vaccine candidates to ensure the likelihood of success to be above 0.8, and this is the point at which the economic benefits of advancing vaccine development and manufacturing capacity are optimised (Michael Kremer, personal communication; for more details, see https://www.AcceleratingHT.org/.87
COVAX is a global collaboration on COVID-19 vaccines coordinated by Gavi, CEPI and the WHO, which aims to secure billions of doses of affordable SARS-CoV-2 vaccines which will be available to all participating nations, securing sufficient supply initially for 3% and then 20% of participating countries’ populations.79 88 89 COVAX aims to secure USD 18.1bn in funding to support the development, procurement and delivery of 2 billion doses of vaccines by the end of 2021. The Gavi COVAX AMC will fund access for lower-income countries. To date 170 nations including 76 wealthy nations, have expressed intent to participate in the scheme, including a UK commitment of £571m.90 Such international collaboration to invest in multiple vaccine candidates reduces the risk to individual countries, strengthens their negotiating position and helps to secure global supplies, reduces the risk that ‘vaccine nationalism’ could reduce availability, and that a bidding war could increase prices,72 81 rendering vaccines unaffordable to LMIC. The participation of a significant number of high-income countries will likely create incentives for others to join the syndicate. If it is politically impossible for all countries to join, informal coordination of initiatives should be pursued (Michael Kremer, personal communication). Furthermore, cooperative allocation of vaccine doses once available is likely to have greater overall health outcomes, in terms of lives saved, than unequal allocation to wealthier nations.91
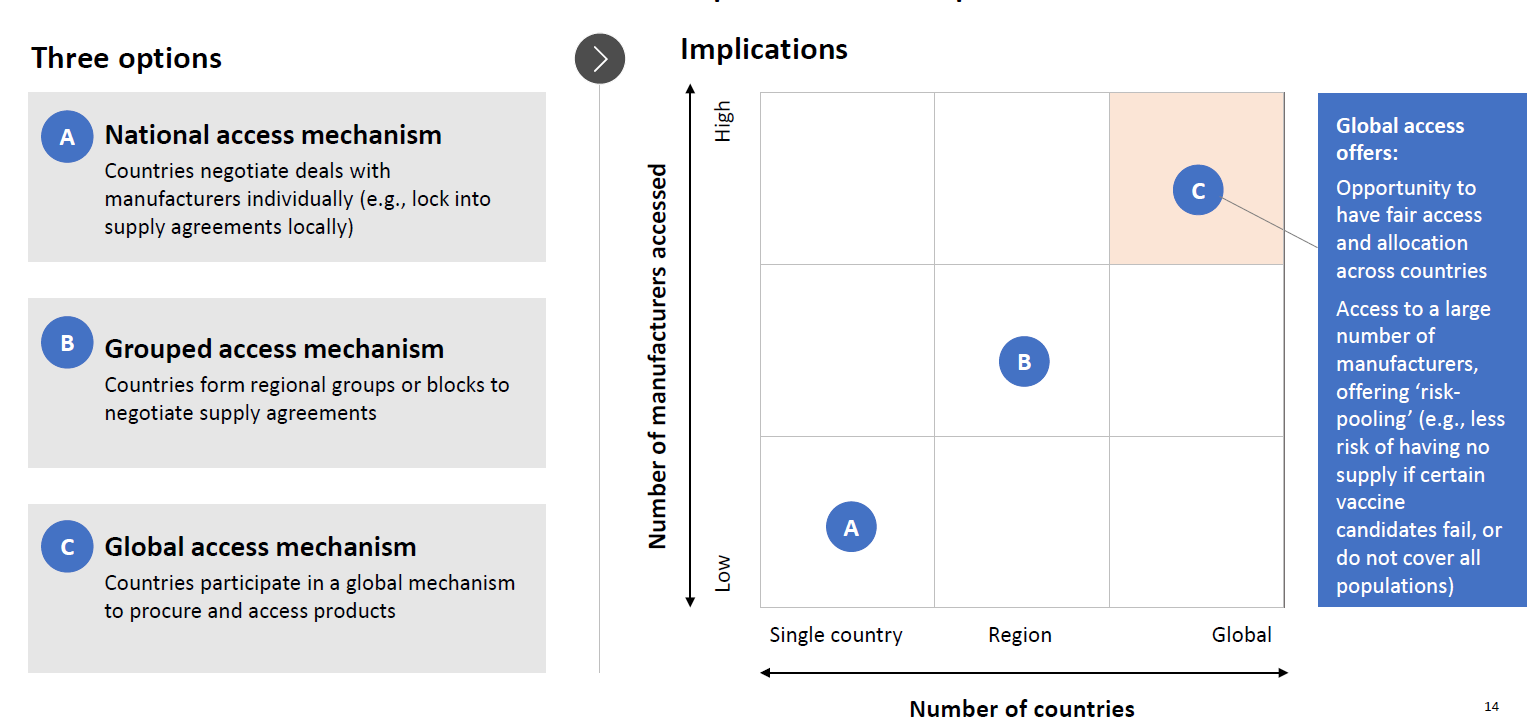
From: WHO Member States Briefing June 2020. A Global Framework to Ensure Equitable and Fair Allocation of COVID-19 products.
Challenges in manufacture of a future vaccine
Once a safe and effective vaccine is available the choice of vaccination strategies will need to be phased to match manufacturing capacity. CEPI estimates that for 2021 a global annual capacity of between 2 to 4 billion doses could be available without disrupting existing vaccine supplies with much of the capacity being in India and China.92 They hope to distribute 2.1 billion doses in 2020/1 and will target high-risk individuals. If immunity is short lived and annual vaccine boosters are needed, capacity will be needed to extend coverage whilst maintaining immunity in existing recipients. A vaccine that confers immunity for less than a year would only be useful in limited circumstances, such as managing outbreaks and in high risk individuals, as the logistics of large scale manufacturing, distribution and use become unworkable for widespread vaccination programmes.
The outstanding issues that need to be established in order to define the manufacturing challenges are:
-
Will we find a vaccine that works?
-
What will the vaccine strategy be?
-
Will the vaccine require single or multiple doses?
-
How long will an immune response be protective and how will a booster strategy work to maintain protection?
-
What process will be used to make the vaccine?
-
What is the amount of the active ingredient (drug substance) per dose?
-
How long will it take to manufacture the required number of doses?
-
What route of administration will be used for the vaccine?
-
How long will it take to distribute and administer the required number of doses?
-
Is the vaccine suitable for worldwide distribution?
UK capacity to develop and make a COVID-19 vaccine
It is clear that worldwide there will be a long lag time to reach a suitable level of sustainable manufacturing.93 With vaccine development normally taking over 10 years and costing 1 to 2 billion pounds, capacity has been built as needed. To build a new biotechnology manufacturing and filling facility can typically take 3-5 years from start to end of commissioning.
At present the UK is constrained in vaccine manufacturing capacity. Because of consolidation of the pharmaceutical industry the UK has capacity to make influenza vaccines and some childhood vaccines but is limited in the availability of sites for further work within the UK. Most of the promising candidates will be taken up by large pharmaceutical companies that are international in outlook. They have the experience of managing large projects and organising large-scale clinical trials, analysing data and registering products. With pharmaceutical companies taking an international view and focussing on a few key production sites for vaccines such as GSK focussing vaccines at Rixensart and Wavre in Belgium there are fewer local facilities with local expertise and capacity.
There are many reasons to make a product on multiple sites; supply security, being close to the user and local knowledge for regulatory issues. However, technology transfer and keeping consistency between sites requires effort and cross cultural understanding. It is feasible that material could be made on a site for one market but not be available for use in other markets because of site registration issues or export restrictions.
To speed up vaccine development in the short term, disposable technology is being used to initiate production using existing facilities that can be repurposed. In the long-term extra capacity will be needed for vaccine supply at a reasonable price. The UK government is accelerating the construction and commissioning of the VMIC at Harwell and has also bought a veterinary vaccine manufacturing facility in Essex (Benchmark). Extra filling capacity has been included in the budget for VMIC leading to a 20-fold increase in capacity. Such investment is made based on assumptions about the most likely type of vaccine to be developed. If the product needs to be frozen, lyophilised, filled into bags etc. the fill lines may need significant modification.
Manufacturing Processes
The type of vaccine is very important for determining what route of manufacture is needed and therefore what type and scale of capacity is needed.93 94 Administration route and storage conditions determine the methods of fill finish, storage and distribution of the product.
Not all platforms under development, such as RNA vaccines, have a proven ability to upscale. More traditional formulations are well established but newer technologies may have a smaller manufacturing footprint and produce many doses rapidly in bulk. COVID-19 vaccines need to be manufactured under current Good Manufacturing Practices (cGMP) in a registered manufacturing facility,94 at high volume, rapidly and ideally at low enough cost to allow affordability and mass immunisation. An overview of the manufacturing process for different vaccine platforms is shown in Appendix 3.
The two leading vaccine candidates developed in the UK are: (1) the chimpanzee replication-deficient adenovirus-vectored vaccine (ChAdOx1) expressing the SARS-CoV-2 spike protein and (2) the self-amplifying RNA (saRNA) vaccine formulated in lipid nanoparticles (LNPs). The ChAdOx1 vaccine developed by the University of Oxford and commercialised in collaboration with AstraZeneca is currently in phase 3 clinical trials.29 The saRNA vaccine is developed by Imperial College London and is in phase 1 clinical trials.29
Besides these two UK-based candidate vaccines, the UK Government also agreed to acquire vaccines from an additional four suppliers from abroad,95 some of which are planned to be manufactured in the UK, as listed in Table 1 below. Thus, in total, the UK Government is planning to source four different vaccine types, from seven different suppliers provided that these complete the trials successfully and obtain regulatory approval. It is worth noting that all of these vaccines target the Spike-protein of SARS-CoV-2, except for the Valneva vaccine where the antigen is the whole SARS-CoV-2 virus in its inactivated state.
Table 1. List of COVID-19 vaccines ordered by the UK Government, subject to clinical success and regulatory approval, listed in the order of their advancement through clinical trials. Table summarise information from a range of sources.29 95 96 97 98 99 100 101 102 103 104 105 106
| Vaccine developer | Vaccine type | Development, testing phase | Million doses ordered by UK Government* | Manufacturing partner | Manufacturing location |
Sources |
|---|---|---|---|---|---|---|
| University of Oxford AstraZeneca | Adenoviral vector | Phase 3 clinical trial | 30 + 70 | Serum Institute of India | India, UK, Netherlands | [29,95,96,97] |
| BioNTech, Pfizer | mRNA | Phase 3 clinical trials | 30 | BioNTech, Pfizer | Germany, USA, Belgium | [29,95,98,99,100] |
| Janssen Pharmaceutical Companies | Adenoviral vector | Phase 1/2 clinical trials | 30 + 22 | Biological E | India | [29,95,101] |
| Novavax | Protein Subunit | Phase 1/2 clinical trials | 60 | FUJIFILM Diosynth Biotechnologies | Teesside, UK | [29,95,102] |
| Imperial College London | saRNA | Phase 1 clinical trials | Not disclosed | Centre for Process Innovation | Darlington, UK | [29,95,103] |
| Valneva | Inactivated viral | Pre-clinical | 60 + 40 | Valneva UK | Livingston, Scotland | [29,95,98,104] |
| Sanofi Pasteur, GSK | Protein Subunit | Pre-clinical | 60 | Sanofi Pasteur, GSK | USA | [29,95,105,106] |
* The first number indicates the million vaccine doses the UK Government agreed in principle to purchase, subject to clinical success and regulatory approval or authorization. When shown, the second number represents the million doses the UK Government could optionally buy, subject to clinical success and regulatory approval or authorization.
The adenoviral vector vaccine platform uses cultured mammalian cells to grow the adenoviral vectors. The RNA platforms utilise a cell-free enzymatic reaction to synthesise the RNA polymer of the vaccine. This RNA molecule is then encapsulated into LNPs (small fat droplets) to prevent degradation and aid the delivery of the RNA into the muscle cells of the human body. The two recombinant protein subunit vaccines are viral proteins produced in large quantities in insect cells. The Novavax vaccine will be formulated using the company’s saponin-based Matrix-M vaccine adjuvant. The whole viral Valneva vaccine is produced by culturing the virus in cells and it is then inactivated with formaldehyde. The downstream purification processes for all of these vaccine production processes in general consist of a series of purification and filtration steps. Details of the production processes for these two vaccine platforms developed in the UK are presented in Appendix 3.
The ChAdOx1 production amounts range between the equivalent of 1500 – 3500 doses worth of vaccine active ingredient (aka. drug substance) per L of culture, depending on the production titres, drug substance amount per dose and losses in the downstream purification. At the 2000 L bioreactor working volume scale, a single batch takes between 26 and 30 days to complete from the beginning of the upstream process to the end of the downstream process, and between 100 – 150 million doses of drug substance can be produced annually at this scale, depending on production titres, amount per dose and losses in the downstream purification.
For sa-RNA vaccines, production amounts range between the equivalent of 2 – 3 million doses worth of vaccine active ingredient per L of bioreaction volume, depending on the production titres, drug substance amount per dose and losses in the downstream purification. At the 5 L bioreactor working volume scale, a single batch takes between 40 and 45 hours to complete from the beginning of the upstream process to the end of the downstream process, and between 5 – 7 billion doses of drug substance can be produced annually at this scale, depending on production titres, amount per dose and losses in the downstream purification.
Challenges in Manufacture
Overall, the challenges in manufacturing are caused by the urgency and scale of the demand for a new vaccine for a previously unknown disease. To address these, rapid-response vaccine production platform technologies have been deployed as these can in principle meet these urgent needs. However, these GMP production technologies are relatively new, and for the RNA vaccine platform there are currently no licensed products on the market. Thus, these technologies were not fully ready and validated to address the current pandemic. Furthermore, clinical trials are not completed thus the final drug substance amount per dose and number of doses required per patient is not yet known, leading to uncertainty and potential changes in manufacturing plans. Due to the pandemic-induced urgency, manufacturers are producing candidate vaccines for clinical trials and are also (in parallel) scaling up for commercial-scale production at risk as trials are ongoing without knowing exactly when and with what outcome trials will complete.
Vaccine supply may be limited by materials or delivery system costs/availability; simple examples are availability of disposable bioreactors, cell culture medium, RNA manufacturing components, glass vials, silicon rubber tubing and syringes and needles. Some vaccines also need an electroporation device to get the vaccine into cells after injection. For the RNA platforms, the material costs are the major contributor to the operating costs and to the overall production costs. The highest cost material is the 5’ cap analogue, for example the CleanCap sold by TriLink Biotechnologies, which is required for the RNA to function in the cells of the human body. All the other production processes, which are either mammalian or insect cell-based, are carried out at a much larger scale, commonly at 2000 L bioreactor working volume. For these cell-based processes, the facility-related costs are the main contributor. Uncertainty with regards to production amounts, rates and costs is caused by uncertainty in the drug substance amount per vaccine dose, production titres, scheduling and production scale.
For the overall vaccine manufacturing process, the bottlenecks could be the fill-to-finish process whereby the drug substance is filled into vials or other containers and the so-called drug product is obtained. Conventional large-scale fill-to-finish technologies can fill up to 400 vials per minute and can operate 60% of the year. Alternative, fill-to-finish technologies such as blow-fill-seal can provide additional filling capacity. Filling in larger containers would speed up the process, and even a 200- and 400-dose IV bag system is developed which can easily cope with the volume and urgency challenges. However, filling in such large containers might be limited by the thermostability of some of the vaccines, such as the RNA vaccines. If RNA and/or other vaccines need to be lyophilised, this would further slow down and decrease the production volumes. The ChAdOx1 vaccine is expected to be filled into multi-dose vials, such as 10-dose vials. Producing for the UK population seems achievable; however production for meeting the global COVID-19 vaccination demand is still an enormous challenge. To meet production targets, single-use technology-based production can be used and scaled out. In addition, using computational modelling together with the vaccine manufacturing processes can substantially improve the performance of these production processes. If the thermostability of the vaccines could be increased, this would translate to larger productivity in the fill-to-finish and reduced supply chain and administration issues.
Supply chain, distribution and administration
There are a number of risks at present. We cannot predict which vaccine candidates will be successful and it should be noted that both of the high profile UK vaccine candidates are based on technology which is promising but not established.
Global supply will need to be rapidly ramped up as production of any SARS-CoV-2 vaccine will add a need for billions of doses of product that was not needed previously. We also need to continue other vaccine manufacture. GSK who are a major vaccine manufacturer currently make about 3 million doses of vaccine a day. That is about 1 billion doses per year or about 1/15th of the quantity needed for COVID-19 but not necessarily available. Similarly, global vaccine capacity for influenza (in 2009) was 900 million doses.69 Substantial components of manufacturing capacity (e.g. - for fill and finish) can be repurposed across vaccines, but not all manufacturing can be repurposed. Global coordination of investment in new plants should ensure the most efficient use of manufacturing capacity.93
The vaccine supply chain consists of: (1) sourcing of raw materials and consumables used for vaccine drug substance and drug product manufacturing, and (2) the distribution of the finished product. In both cases, the supply chain consists of a series of transportation and storage steps.107 The sourcing of material and consumables as well as the distribution and administration of vaccines might be disrupted by the pandemic itself if and when borders are closed, or transportation and travel is restricted, personnel become ill, raw material or consumable manufacturing facilities underperform or close down, countries compete for resources in short supply and the medical system is overwhelmed with treating patients and cannot allocate enough personnel and resources to vaccinate the population.
The International Air Transport Association recently reported that 8000 Boeing 747 cargo loads would be needed to distribute a single dose of vaccine to 7.8 billion people. Frozen vaccines would be more difficult to transport because of lack of suitable carrying capacity.107 There is currently uncertainty around the thermostability of these vaccines, especially the newer vaccine types such as the RNA vaccines. It is possible that RNA vaccines would need to be transported and stored at -80°C throughout the distribution chain. The distribution of vaccines at very low temperatures, such as -80°C, is extremely challenging or even impossible in low and middle income countries with hot and/or humid weather conditions where road and/or electricity infrastructure is lacking. For all of these vaccines, manufacturers and researchers are working towards improving thermostability to reduce the need of the distribution at very low temperatures.
Finally, using the currently available qualified medical staff for vaccine injection into patients, the overall bottleneck of the entire manufacturing-supply-administration chain appears to be the final administration step. To address this administration challenge, additional staff will need to be trained (e.g. pharmacists, midwives, physiotherapists, dentists and vets) to immunise the population rapidly and safely.108 In principle, vaccination campaigns can also be designed to maximise the number of individuals vaccinated per medical staff per unit time. All of the seven vaccines to be acquired by the UK government are administered intramuscularly; however, these might require two doses in a prime and boost regimen thus requiring even more medical staff and resources.29
Advantages of an integrated manufacturing-distribution-administration chain
The vaccine manufacturing-distribution-administration chain represents a complex system with multiple parts and multiple objectives which are sometimes competing, such as maximising distribution speeds, maintaining the stability of the vaccine product, maximising vaccination coverage and minimising costs. Mathematical optimisation algorithms will be instrumental in designing and operating such complex systems. By developing and using such methods, the entire system might be operated at its maximum potential. In parallel to this, epidemiology modelling can be used to predict COVID-19 disease spread and minimise COVID-19 related mortalities.109 Coupling these two models and using them in real-time with data from the underlying physical processes, could help combat the current COVID-19 pandemic more effectively in the UK and beyond.
Lack of access to vaccines may exacerbate health inequalities in the UK and globally
There are a number of issues that need to be considered around the impact of COVID-19 vaccine programmes and how they are rolled out on health inequality.110 These can be split into those that impact health inequalities in the UK and those that impact health inequalities globally. They can be further split into those that are direct effects of the vaccine programme versus those that arise as opportunity costs of the vaccine programme. We briefly address each in turn.
Given that it is likely that at least in the immediate term the demand for the vaccine will outstrip supply there will be questions about who is given priority access. It is important that these questions are resolved in fair, transparent and accountable ways employing appropriate processes to do so.111 Thinking first about the various scenarios outlined for vaccine roll out in the UK it is apparent that there will be different sets of winners and losers in each scenario. When choosing between scenarios these winners and losers should be identified for example old versus young, rich versus poor, white versus ethnic minority. Existing health inequalities between these groups should be taken into account when deciding which of the scenarios to pursue in terms of their impacts on exacerbating or ameliorating existing health inequalities. Clear criteria should be defined to judge the relative merits of the different scenarios and clear justification for why a given scenario is chosen over others should be made explicit.112 It is important to recognise that vaccines are one element in the portfolio of tools that can be used to tackle COVID-19. As vaccines become available the allocation of resources and efforts across different elements in this portfolio will change. This change in mix of strategies will give rise to winners and losers.
It is also important to consider the opportunity costs of the vaccine programme when thinking about impacts on health inequality. A vaccination programme will use resources that would otherwise have been used to deliver other services to the population. Thinking about what services will be displaced, the loss in health arising from this displacement and identifying the groups that will incur this loss in health are important considerations from a public health and inequalities perspective. Some of this displacement will be direct such as the use of medical supplies (e.g. syringes) that will be used on the COVID-19 vaccine which might disrupt vaccination programmes for other diseases. Indirect effects will include the time health care workers spend on delivering vaccines that would otherwise be used to deliver other healthcare. Thinking about the impact of this broader displacement is also valuable to ensure policies that are chosen improve population health and wellbeing overall and reduce health inequalities.
Other key within-country considerations include the impacts of existing inequalities in supply of healthcare workforce.113 Poorer parts of the population suffer from worse health in the UK and are currently underserved in terms of access to primary care. If existing primary care infrastructure is utilised to deliver COVID-19 vaccines this primary care supply inequality may result in reduced access to the vaccine in poorer areas due to lack of human resources to deliver the programme in these areas. These implementation issues should be carefully thought through if health inequalities are not to be exacerbated by any vaccine programme.
Finally, questions of whether it will be possible to purchase vaccines privately outside of the programme is also an important consideration. If wealthier individuals can bypass the chosen national prioritisation scenario, this will have implications for health inequalities both in terms of how many vaccines are available in the public sector as well as in terms of health inequalities arising from the distribution of vaccines.
There are a number of ways that the UK’s decisions on vaccines can impact global health inequalities. Some of the most obvious of these include the fact that any vaccines and associated medical supplies bought by the UK will not be available for use in other countries. Competition for vaccines amongst countries may drive prices up globally, pricing them out of reach of many poorer countries. These impacts may go beyond COVID-19 vaccines and also impact supplies of key medical equipment used to deliver these vaccines that are also used in the delivery of other healthcare. Other considerations are those based around intellectual property and patents. Strict enforcement of pharmaceutical licencing backed up by international trade rules such as TRIPS (Trade-Related Aspects of Intellectual Property Rights) have in the past been seen as restricting access to healthcare from those who need it most in order to serve the financial interests of the pharmaceutical industry.114 A particularly striking recent case study is that of antiretroviral drugs in South Africa.115 Careful consideration should be given to the issue of access to healthcare globally when engaging in licensing agreements with vaccine manufacturers and participating in collective purchasing agreements with other governments. World Health Organization initiatives to ensure equitable access for all globally provide valuable opportunities to collaborate with other countries to promote health equity.89
4. Ensuring the success of a vaccination programme: vaccine acceptability
-
Safety, tolerability, effectiveness and routes of administration may influence vaccine acceptability
-
Clear communication is needed to build trust in vaccine benefits to maximize acceptability and thus effectiveness
-
Barriers to vaccine uptake need to be minimised
-
Priority groups will often require dedicated focus accounting for specific needs and concerns
Safety, tolerability, effectiveness and routes of administration may influence vaccine acceptability
The first vaccines that are licenced for use against COVID-19 are likely to significantly influence the public perception and debate. There is a risk that a vaccine that is poorly effective or reactogenic, or which requires multiple booster injections will not create an incentive for uptake among those who perceive themselves at low risk, and if the vaccine is perceived as having been rushed through safety testing, this might create long term distrust and hesitancy.116 117 118 119
Clear communication is needed to build trust in vaccines, increase acceptability and thus effectiveness
Vaccines and vaccination programmes need to be trusted to maximise participation in any national vaccination programme. Clear, transparent communication can be used to address rational doubts and to enable informed decision-making. Such communication should include information on the benefits of any vaccine to individuals and their close contacts and community; it should not hide the potential limitations of vaccines including possible limited availability, incomplete protection requiring boosting and reactogenicity.37 120 121 122 While such negative or complicating factors might lower uptake, their discovery post-rollout is likely to have a far greater negative impact on uptake. One important aspect of vaccination to be communicated clearly and early, and involving public dialogue, is how and why groups will be prioritised for vaccination, so that communities and individuals are supportive when vaccines are rolled out in a staggered manner.
Effective communication programmes can benefit from using previously validated approaches. For example, the 3 E’s (Explanation, Engagement and Education) approach is used by the Bank of England to address the ‘twin deficits’ of public understanding and trust.123 124 125 Involving widely trusted individuals with broad reach, such as healthcare professionals particularly in primary care, can help to manage expectations and anxieties.37 Approaches such as the 3 E’s require a thorough understanding of communities’ beliefs, values, power structures and behaviours in order to be effective, as was seen when tackling a polio outbreak in Somali pastoralist communities in 2013-14.126
The vaccine hesitancy seen for many non-COVID-19 vaccines is very likely to also occur for any COVID-19 vaccine.127 Some hesitancy is based on rational concerns, which can be addressed through clear communication and dialogue,128 however people may have a range of concerns or fears. One framework for understanding vaccine hesitancy uses two axes: one considering the level of trust individuals and groups have in health authorities; the other considering people’s commitment to managing risk in their lives in general, and their own health in particular.129 Those who take control of their health but distrust authority are likely to rationalize their hesitancy, while those who do not are more likely to simply avoid the issue as far as possible. The varied reasons for vaccine hesitancies will require alternative strategies that meet individuals where they are. One example of such an approach is ‘convert communicators’, where those with previously strongly held opinions explain why they previously held that position and provide new information that caused them to change their mind.130 131
Barriers to vaccine uptake need to be minimised
Smooth supply and availability of vaccination is needed to ensure the success of a population-wide vaccination strategy. This will require addressing social and economic disincentives to vaccination, such as the need to take time off work or secure child care to obtain a vaccine; such barriers are likely to be greatest for those in society most vulnerable to COVID-19. This can be achieved through local distribution involving community workers (not just health workers) where available, with evening and weekend opening hours. Charging for vaccination, or withholding vaccines based on citizenship, will lower population-level vaccine effectiveness and should therefore be avoided. Involving community leaders in vaccine campaigns is likely to help to maximize uptake by addressing religious, cultural or other context-specific concerns about vaccine uptake.
A further step to reducing barriers would be to mandate vaccination as a prerequisite for resuming activities of various kinds. For example, vaccination could be mandatory for health care workers to engage in certain activities as has been used in some settings, for example, with influenza and hepatitis B vaccination.128 132
Priority groups will often require dedicated focus accounting for specific needs and concerns
Some high-risk groups have particularly high barriers to vaccine uptake. In general, priority groups are likely to be those at greater risk of (i) infection; (ii) transmission; or (iii) poor health outcomes. Maximizing vaccine uptake in those who perceive their risk to be low, such as young adults, might be enabled by a focus on the benefits of such vaccination to people they care about who are at greater risk of poor outcomes – for example, older aged relatives. Ensuring such older individuals are vaccinated is likely to require different messaging, perhaps linking COVID-19 vaccine to existing annual influenza shots that over-65s are routinely offered.
Ethnic minority groups have been disproportionately impacted by the COVID-19 pandemic in the UK in terms of both acquisition and outcome risk. As scientists work to create a viable vaccine it will become extremely important for this population to have adequate access and high uptake. Studies have shown that immunisations in the UK are well received, but there is evidence that uptake of some immunisations are lower in Black and Asian minority groups.133 Cultural belief differences as well as cultural mistrust are major obstacles in the implementation of vaccine and immunization promotion.134 There is a long history of minorities being mistreated by the healthcare system which reduces their participation. Physician communication behaviours have been shown to have different effects on patient trust depending on the race of the patient.135 While cultural mistrust may deter ethnic minorities from going to their general practitioner, lack of culturally sensitive communication limits the public health information they receive. Health guidance communication only given in English reduces the participation in immunization among children from ethnic minority backgrounds due to language barriers.134 Overcoming these barriers will require collaboration with patients and their families to ensure that ethnic minority populations have access to vaccinations.136
5. Requirements and consequences of vaccination programmes, possible scenarios
-
Once vaccines have successfully completed clinical trials, decisions will need to be made as to the most appropriate vaccination strategies
-
Suitability of a vaccine for different strategies will depend on the properties of the vaccine itself and its availability
-
Considerations include whether a vaccine prevents disease or transmission; efficacy in different recipients; requirements and suitability for multiple doses or boosters; affordability; constraints in manufacturing capacity and supply; and acceptability.
-
When vaccine supplies are limited, priority could be considered for those most at risk of severe disease, health and social care and other key workers.
-
The longevity and nature of protection elicited by any vaccine will have a significant impact on immunity generated, our ability to predict likely waves of infection, the numbers of doses that need to be produced and administered (which in turn influence vaccine affordability), and feasibility of distribution, public acceptability and uptake.
-
Decisions at first will need to be made on limited information
The first generation of vaccines for SARS-CoV-2 may be available within the next 6-18 months. However, these may be suboptimal. Furthermore, a vaccine may be developed but not available to the UK as a priority. Decisions on which vaccine strategies to adopt will depend on the availability of a vaccine, the immunity elicited and acceptability of the vaccine.79 137 138 139 140 Different vaccine strategies will have different results; immunity in vulnerable populations and those at high risk of exposure, or reduced transmission or elimination of the infection in the population at large. The effects of vaccination in different groups such as children, clinically vulnerable groups and older people must be considered. All vaccine scenarios discussed below are examples, are not mutually exclusive and are likely to occur in conjunction with continued non-pharmaceutical interventions.
Current clinical trials are designed to test efficacy in reducing clinical disease (symptomatic infection) and the FDA has stipulated a requirement for 50% efficacy for licensure;40 trials are not necessarily designed to detect protection against infection, severe disease, transmission, or efficacy in different groups, although these may be measured as secondary outcomes. A vaccine with low efficacy will reduce disease burden, but is less likely to be successful in reaching herd immunity. Further information, for example, on the longevity of immunity and requirement for boosters, may be limited at the time when the first vaccines are used. Long term safety monitoring will be essential.
This will necessitate a flexible approach, in which vaccines are evaluated as they complete clinical trials, and vaccine strategies adapted on an ongoing basis. This should be supported by modelling studies to determine optimal vaccination strategies as information emerges on vaccine properties and availability.138 139 140 As vaccine strategies develop, this will require clear open communication with the public and health care workers.
Scenario 1: Vaccination of groups most vulnerable to severe disease
| Who | Properties of vaccine | Viral circulation | Doses needed (UK) Estimates based on 2 doses, 15% wastage |
Advantages & Limitations |
|---|---|---|---|---|
| Groups at most risk of severe disease | Effective at preventing severe disease in high risk groups. | Virus continues to circulate. | Examples: 5m doses (2.2m clinically extremely vulnerable in UK)[141] 29m doses (12.5m UK over 65s)[142] 60m doses (25.5m UK over 50s) |
Potential for large reduction in disease burden for relatively low number of doses. Some vaccines might be of low efficacy in older people. Not all those at high risk can be identified. |
In Scenario 1,141 142 vaccines would be administered to those at most risk of severe disease. This would require fewer doses than a strategy of widespread vaccination, and is likely to be the optimal strategy when vaccine supplies are limited.65 143 Decisions will need to be made as to who should be within the priority groups for vaccination according to efficacy and availability.79 137 The UK Joint Committee on Vaccination and Immunisation (JCVI) has issued interim advice that this could include those over 50 and with other risk factors, such as chronic heart disease, chronic kidney disease, chronic pulmonary disease, malignancy, obesity and dementia.144 The WHO initially recommended prioritisation of people over 65, adults between 30 and 70 suffering from cardiovascular disease, cancer, diabetes, obesity or chronic respiratory disease, as well as health care workers.137 Priority groups could also include those in the clinically extremely vulnerable group, who have been shielding, pregnant women and those who are immunosuppressed,144 but only if the vaccine can be safely used in these groups. The vaccine should ideally be effective at preventing severe disease in a high proportion of those in the high-risk groups such as older people, who often respond poorly to vaccination. Prevention of infection itself and transmission reduction, although desirable, are not necessary. Long-lived protection is also a lower priority than under other scenarios, although a requirement for multiple doses or frequent boosters will make a vaccination programme more difficult and costly to implement. In the longer term this will require an ongoing programme of vaccination of anyone who enters risk groups.
This scenario means that the virus continues to circulate. Not everyone who is at risk of developing severe disease can currently be identified based on pre-existing risk factors, leaving some individuals vulnerable. If the vaccine is only partially protective, protection will be difficult to confirm in an individual in the absence of clear correlates of protection.
Scenario 2: Vaccination aimed at reducing incidence in those at high risk of infection
| Who | Properties of vaccine | Viral circulation | Doses needed (UK) Estimates based on 2 doses, 15% wastage |
Advantages & Limitations |
|---|---|---|---|---|
| Those at high risk of infection | Prevents disease in healthy adults | Virus continues to circulate. | Examples 7.5m doses (3.3m UK health and social care workers) 17m doses (7.3m other key workers)[145] |
Not all those at high risk can be identified. |
In Scenario 2,145 the strategy aims to protect those at the highest risk of infection to reduce the incidence of disease. Those in occupations at high risk of exposure, particularly health care workers could be prioritised. Priority might be extended to key workers, such as emergency services and teachers, and occupations at high risk of exposure 64 137. The vaccine does not need to be effective in vulnerable groups, and protection may not need to be long lived although a requirement for frequent boosters will be more difficult and costly to implement. The historically low uptake of vaccines, such as the seasonal influenza vaccine, and reasons for vaccine hesitancy among health care workers would need to be addressed if uptake were low 146. There is precedent for an expectation of vaccination of healthcare workers in the NHS who are restricted in the procedures they can carry out if they are not vaccinated against Hepatitis B. The virus will continue to circulate in the wider population and pose a risk to the vulnerable.
Transmission to those in high risk groups may be reduced by vaccination of health and care workers by creating a cocoon which protects the vulnerable. In our recent report, we estimate that early in the pandemic, at least 10% (CI 4-15%) of all COVID-19 infections in England were among these groups, with 6% of infections among care home residents.147 Vaccination of care home staff against influenza has been shown to significantly reduce mortality.148 A significant proportion of transmission events are likely to occur within households. Therefore, if transmission is reduced by vaccination, it might be extended to those who share households with those in vulnerable groups. 74% of clinically extremely vulnerable (CEV) people live with other people (in the UK), and 15% live in a household with children aged under 16 years.141 However, it will be difficult to identify and prioritise all contacts of the vulnerable.
Although most vaccines that prevent disease also prevent transmission of infection, there is the potential that a vaccinated individual will still shed virus if infected. The effect of a vaccine on transmission will not be available following the first trials of SARS-CoV-2 vaccines. Vaccines which prevent disease while not reducing viral shedding, or which do not protect all recipients, could result in inadvertent transmission, particularly if behaviour changes in those who have been vaccinated.
Scenario 3: Vaccination of wider population
| Who | Properties of vaccine | Viral circulation | Doses needed (UK) Estimate based on 2 doses, 15% wastage. |
Advantages & Limitations |
|---|---|---|---|---|
| Whole population or large sectors of the population with eventual aim of achieving herd immunity [149,150] | Ideally generates long lived immunity in high proportion of recipients. Vaccine platform must be scalable. |
At first the virus continues to circulate, but transmission may be reduced. As herd immunity is achieved circulation is reduced. Virus eventually eliminated from most of the UK. Sporadic outbreaks may still occur in those not protected by vaccine |
Very large number of doses depending on efficacy. Example: 123m doses (80% of UK population of 67m) |
Doses needed might exceed initial availability (see Table 1). Must be widely acceptable and available. |
Under Scenario 3, the vaccine is offered to the whole population or large sectors of the population.149 150 A widespread vaccination programme would eventually aim to achieve herd immunity, in which a sufficient proportion of a population is immune to prevent sustained transmission of an infection. This strategy would reduce the incidence of infection overall and thus in addition to reducing severe disease, would reduce the potential long-term effects of milder SARS-CoV-2 infection which are still unknown.
For widespread use, the WHO recommends a vaccine product profile of at least 50% efficacy in the wider population, preferably 70%, with consistent protection shown in the older people.62 118 A widespread vaccination policy could substantially reduce disease burden, even in the absence of herd immunity. A recent model suggested that, assuming immunity lasts at least one year, over 50% of deaths could be averted with as little as 35% of the population vaccinated if a vaccine has more than 50% efficacy 65. Once a vaccine is widely available and assuming sufficient vaccine efficiency, widespread vaccination, particularly of high-transmission groups may prove to be a more efficient strategy to minimise deaths and hospitalisations than targeting vulnerable groups,65 140 143 however, this is dependent on our ability to identify and prioritise those driving transmission events, for example, the role of children in SARS-CoV2 transmission is still unclear.151 152
To achieve herd immunity, a suitable vaccine must provide sufficient immunity in those vaccinated to reach an immunity threshold within the population. Estimates of the proportion of the population that would need to be immune to achieve herd immunity vary.153 Vaccine induced immunity will be in addition to naturally acquired immunity following infection. For SARS-CoV-2, estimates of R0 vary, however (based on 1-1/R0) the proportion of the population that would need to be immune to achieve herd immunity has been estimated as 50-80%, although herd immunity may be achieved at a lower rate of immunity, for example if it exists in those more likely to transmit infection and depending on behaviours.139 154 155 A recent model suggested that the epidemic might be constrained if 50% of the population is vaccinated, in addition to naturally acquired immunity, if that vaccination is optimally targeted for example to those most likely to be onwards transmitters; however in reality optimal strategies are unlikely to be achieved, as those transmitting cannot be easily identified and selectively prioritised.65
This strategy requires a vaccine to be available in a large number of doses. The UK government has agreements to secure hundreds of millions of doses of vaccine from different suppliers (Table 1), however, not all vaccines currently in trials will prove to be effective or available in the short term. The longevity of immunity is important to ensure sufficient levels of immunity can be achieved over the course of a population wide vaccination programme, although boosters may be required to maintain immunity. As we discuss earlier in this report, a partially protective vaccine will require a higher proportion of the population to be vaccinated to achieve the same levels of immunity. Furthermore, the response to any vaccine is likely to be heterogeneous. Potentially, therefore the virus would continue to circulate, as immunity may be induced in too low a proportion of recipients or be too short lived to achieve herd immunity, however the extent and frequency of outbreaks would be expected to decrease.63 156 157 Even if herd immunity is achieved, outbreaks could still occur for example, in social groups or geographical regions of low uptake or as immunity wanes.
Those at low risk of severe disease may have a lower uptake of the vaccine especially if it is poorly effective, requires boosters or is reactogenic. Widespread uptake may depend upon a vaccine being perceived as having a low risk-and-adverse-effects to benefit ratio in those at low risk of severe disease. Uptake must be encouraged to achieve the required levels of coverage in those at low risk of severe disease to protect those who cannot be vaccinated or who respond poorly and are likely to remain vulnerable to infection or disease. If the vaccine is partially effective, correlates of protection are unknown and therefore protection cannot be tested for, widespread vaccination could lead to increases in risky behaviour in those who assume they are protected.118
Even once high levels of immunity are achieved in the population, surveillance must be maintained as there is a risk that the virus could be re-introduced if still circulating globally allowing outbreaks to occur. Sustained transmission may occur when the number of susceptible people increases sufficiently, for example, if immunity wanes, if coverage is uneven and herd immunity is not achieved due to poor uptake, or in the longer term if mutation of the virus allows it to evade immunity. Only the eventual goal of global eradication or control will ensure the low risk of outbreaks in the UK.
Scenario 4: Vaccination in response to local outbreaks
| Who | Properties of vaccine | Viral circulation | Doses needed (UK) | Advantages & Limitations |
|---|---|---|---|---|
| Wider community following outbreak | Must induce very rapid protection against disease or transmission. | Could reduce the extent of local spikes in transmission following an outbreak. | Sufficient doses must be immediately available. | Requires active regional surveillance. May be used in conjunction with locally increased stringency of NPI. |
In Scenario 4, members of communities are vaccinated in response to outbreaks due to the higher risk of transmission events in the wider community following a spike in cases. For example, Hepatitis A vaccination can be employed following localised outbreaks.158 Scenario 4 might be used once vaccination is more widespread in a population, if immunity wanes or coverage is low in certain populations, allowing sustained transmission to occur. The vaccine itself would ideally prevent both transmission and disease, but crucially must induce immunity sufficiently rapidly to protect before the outbreak has spread through the community. The WHO recommends immunity must be induced in less than 2 weeks and ideally following a single dose to be suitable to contain outbreaks.62 Immunity induced by the vaccine could be short lived if it is sufficient to contain the outbreak. Sufficient doses would need to be available locally as part of a rapid response. Success would require continuous and effective testing and community engagement. Given the short serial interval of SARS-CoV-2 transmission and pre-symptomatic transmission, attempts to trace and vaccinate only direct contacts and their contacts (ring vaccination) is unlikely to be effective in containing outbreaks and immunisation of the wider local community likely to be a more effective strategy.
6. Long-term lessons and preparedness
-
Global coordination of vaccine purchase, production and distribution is needed
-
Vaccine availability, uptake and effectiveness in different populations under different vaccination programmes should be monitored
-
Different vaccination strategies should be adopted and reviewed on an ongoing basis as data on effectiveness and longevity of immunity emerge and new vaccine candidates become available.
-
Long-term safety following widespread use should be carefully monitored
-
Viral evasion of vaccine-induced immunity by mutation may require modification of vaccines but may be avoided by inclusion of multiple targets or conserved regions of SARS-CoV-2 in vaccines
-
Public expectations of access to and effectiveness of a vaccine should be carefully managed
-
Financial incentives should support development of second generation vaccines that are more effective, affordable and acceptable
-
Global collaboration to invest in research, training and infrastructure needed for successful vaccine programmes will support long term preparedness
Long-term effectiveness and safety of vaccines in different populations should be monitored
Individuals receiving vaccines will need to be monitored for longevity of immunity and efficacy in clinically and geographically diverse populations to establish the overall effectiveness of first generation vaccines.118 159 Furthermore, if different vaccines are suitable for use in different populations or more than one vaccine needs to be used in combination, this will require coordination of the manufacturing and supply chains.
Post-licensure (phase IV) monitoring will be required to identify longer-term adverse events, including those that might be associated with waning of immunity and immunopathology. Rare adverse events or limited effectiveness in the field may only come to light when very large numbers of people are vaccinated.
As immunity builds in the population as a result of naturally-acquired immunity, use of therapeutic monoclonal antibodies, or through vaccination, viruses that mutate so as to be less well recognised by and evade the immune system may have a selective advantage and become the dominant strain, potentially reducing the effectiveness of any vaccine. SARS-CoV-2 mutates less frequently than some other viruses which use RNA as their genetic code (such as influenza) because coronaviruses possess a genetic proof-reading mechanism 160 161 162. Changes to the genetic code of a virus can come with a fitness cost, for example, in terms of ability to replicate and transmit, and therefore immunity within the population must be above a certain threshold to drive selection of otherwise detrimental mutants 156. As not all parts of the virus are able to mutate without detriment to the virus, if these regions are also the target for vaccine induced immunity, viral evasion of immunity may not occur. For the moment, there is no evidence that SARS-CoV-2 is undergoing changes in its genetic code that will significantly change its recognition by immunological memory responses induced by current vaccine candidates 162. However, other CoVs show substantial genetic variability 163 164. Studies that use pseudovirus in culture have shown the potential for loss of recognition of the SARS-CoV-2 spike protein by antibody following mutation, although this was prevented if antibody recognising more than one part of the spike protein was present 165. Vaccines that induce immune responses to multiple parts of the spike protein or vaccines containing more than one viral component may protect against variants of the virus. Vaccine manufacturers will need to be able to respond to the discovery of any temporal or geographical variation in circulating virus and rapidly reformulate better matched vaccines if this becomes necessary.
A coordinated global vaccination programme and support for development of second-generation vaccines is needed
It is in the long term interests of sustaining international travel and trade that efforts to contain COVID-19 are made on a global scale. Cooperation between nations to invest in vaccine development, manufacture and purchase will increase the chances of successful development and availability. Furthermore, allocation of vaccine doses, once available, to all nations collaboratively is likely to save more lives than unequal allocation of the same number of doses to a limited number of nations 91 143.
If the first vaccines developed are sub-optimal, second generation vaccines will be needed which are more effective, cheaper, give longer-lasting immunity and/or are more acceptable (in terms of reactogenicity/routes of administration) and therefore more suitable for widespread use. The development of multiple vaccine candidates increases the likelihood of availability of vaccines with potentially different characteristics. This will be particularly important while information is lacking on how long protection following vaccination lasts.
Investment in and deployment of the initial vaccines may mean that the development of second generation vaccines is delayed or disincentivised. Until correlates of protection are identified and the level of effective immunity clearly established, large studies will be needed for every new vaccine to prove superiority of protection in the wider population. This will add to the costs and difficulties of developing next generation vaccines, particularly if disease incidence has been reduced to the levels where very large population studies (of the order of tens or hundreds of thousands of participants) would be needed to prove efficacy.
The race today is to make a vaccine, any vaccine with cost not being a major consideration. However as time progresses governments will want a cost effective vaccine. To date Moderna are thought to be targeting USD 50 to USD 60 per course (USD 25 to USD 30 per dose), Biontec/Pfizer USD 19.50 per dose and AstraZeneca a few dollars per dose.166 To use the Moderna vaccine for one cycle of vaccinations in the UK would cost about USD 3.4-4 billion just for the vaccine. Even a few dollars a dose will be out of reach for much of the world’s population. As the memories of the economic cost of our recent shutdowns recede there will also be significant pressure to reduce annual re-vaccination costs if they are necessary so a second round of more cost effective vaccines may be needed. In LMIC the ability of the vaccine to be integrated into existing vaccination programmes and infrastructure will determine its affordability.76
Sustained funding will ensure that no one vaccine company develops a monopoly and will maintain an incentive for market entry of new vaccines. Such sustained investment will require political will and global collaboration. International collaboration whereby each country has a share in many vaccine candidates will reduce the risk to individual countries that the vaccines they invest in will fail. Lack of monopoly and negotiation for purchase of supplies at a lower price will ensure global affordability and distribution of a vaccine. Globally coordinated upscaling of manufacturing will insure sufficient capacity, reduce the likelihood of ‘vaccine nationalism’ and help to ensure availability of affordable global vaccine supplies, thus reducing the likelihood of future global outbreaks.
Investment in vaccine R&D, global organisation and public perceptions of vaccination will aid pandemic preparedness, UK plc and support global health in the long term
Following the Ebola virus outbreak, global calls for an international fund for vaccine development led to the establishment of the Coalition for Epidemic Preparedness and Innovations (CEPI), formally launched in 2017, with the remit of developing vaccines for priority pathogens and improving preparedness for outbreaks of infectious diseases 167 168 169 170. In the long term, sustained global collaboration will ensure we are capable of responding to future outbreaks as part of an integrated international pandemic response, but investment is also needed in local health care provision and community engagement 171. Lessons must now be learned from the SARS-CoV-2 pandemic in order to prepare for the risks of future outbreaks.
During the COVID-19 pandemic, vaccines have come under scrutiny as never before. Public perceptions of the safety and effectiveness of vaccination will be shaped by the success or otherwise of the development and implementation of SARS-CoV-2 vaccination programmes. Premature licensure and implementation of a vaccine programme is likely to negatively affect public perceptions and subsequent uptake of future vaccines, if the vaccine proves ineffective or to have substantial side-effects. On the other hand, a successful programme offers an opportunity to increase public engagement with vaccination more widely.
The UK response to the current pandemic has proven its place as a global leader in the development of vaccine technology. Investment can be made at a national level and new funding instruments such as advanced market commitments could be used to incentivise investment in vaccine development and manufacturing facilities via international organisations.
In the long term, both ‘push’ and ‘pull’ financial instruments will be needed to maximise the likelihood and expedite the success of vaccine programmes. A criticism of push funding, which invests in basic research and development costs ex-ante, is that there is a risk of investing in candidates and research with a poor chance of success, with the risk of failure taken entirely by the funder. Furthermore, it does not incentivise speed and efficiency of research. Pull funding can be used to reward both the development of the final product, and for achieving innovation, goals or milestones relating to health.73
To deploy vaccines faster for future outbreaks, the clinical trials and the regulatory approval process should be further accelerated, and surge vaccine manufacturing capacity should be maintained. Completing clinical trials and gaining regulatory approval is a major bottleneck as this currently is estimated to take around 12-18 months, even with fast-tracking. This can in principle be further accelerated by complementing a vaccine manufacturing platform, such as the RNA platforms, with a Quality by Design (QbD) modelling framework which incorporates disease-agnostic prior knowledge. This could in principle serve as a “pre-qualification” to speed up clinical trials and the regulatory approval process, also in case of a new outbreak caused by a new pathogen.172 Maintaining surge vaccine manufacturing capacity is also crucial for rapid-response vaccine production. This would be comparatively easily achieved for the saRNA platform as it can produce high vaccine volumes, rapidly at a small production scale in small facilities, that can also operate on single-use production equipment, thus would be financially low cost to maintain. These facilities, when there is no outbreak, instead of being idle, could also produce other high-demand vaccines or vaccine candidates for clinical trials. Switching between vaccines against different diseases would be relatively straight-forward when single-use production equipment is used.
The investment and scientific innovations that have been made in vaccines during the pandemic will benefit the development of future vaccines. For example, there is a pressing need for the development of a universal influenza or coronavirus vaccine that will protect against emerging pandemic strains. Sustained investment in basic science and novel vaccine platforms will shorten future development times for novel vaccines. For example, rapid sharing of the genetic code of the SARS-CoV-2 virus and its use to develop novel vaccines occurred in record speed, due to the technologies developed as a result of investment in basic science.173 We need a better understanding of the transmission, disease mechanisms and immune response to infections, and investment in the development of effective vaccine technologies, particularly in the light of an aging global population. Continued investment should support the training and careers of personnel with expertise as well as infrastructure, in the following areas;171 174 175 176 177
-
Pathogen surveillance and discovery
-
Basic science relating to infectious diseases and development of novel vaccines
-
Pre-clinical and clinical testing of vaccines and novel vaccine platforms
-
Population scale monitoring and measuring of vaccine effectiveness and adverse events
-
Vaccine manufacturing; skills training, facilitation of technology transfer and scale up
There are still many challenges in the field of vaccinology. Such investments combined with financial incentives, will not only provide long term preparedness for future global pandemics but will facilitate development and success of vaccines for existing infections which are desperately needed to improve global health.178 179 180
Acknowledgements
The Institution of Chemical Engineers (IChemE) and the UK chapter of the International Society for Pharmaceutical Engineering (ISPE); Zoltán Kis, Kyungjae Tak, Dauda Ibrahim, Maria Papathanasiou, Benoit Chachuat, Cleo Kontoravdi and Nilay Shah, Imperial College London.
Appendices
Appendix 1 Human challenge studies
Background
Several experts in epidemiology, immunology, public health and bioethics have argued or proposed that controlled human challenge trials of candidate SARS-CoV-2 vaccines be seriously considered. In brief, a human challenge trial of a candidate SARS-CoV-2 vaccine would involve the intentional infection of a small number of healthy volunteers with SARS-CoV-2; some of these volunteers would have received the vaccine, and some would have received a placebo. Eyal, Lipsitch and Smith57 were among the first to argue that such human challenge studies could, through bypassing conventional Phase 3 trials of candidate vaccines, subtract many months from the licensing process, making effective vaccines available much more quickly. Jamrozik and Selgelid58 argue that, in addition to this, human challenge studies could enable the rapid and accurate comparison of several candidate vaccines, simultaneously, whereas attempting this in Phase 3 trials would ‘plausibly require tens of thousands of participants, and take many months or years to complete’. As these papers point out, there are also important risks to consider, in human challenge studies: for example, the direct health-risk to participants (which should be minimized by restricting volunteers to healthy young adults), the risk of undermining public confidence in vaccines (in the event of untoward effects of the human challenge studies), and the risk of infection of third parties such as researchers (which should be minimized by protective measures).
On 6th May, the World Health Organization published a report181 conditionally backing human challenge trials of candidate COVID-19 vaccines, subject to certain criteria being met. The report states the following:
‘Challenge studies might be particularly likely to accelerate the availability of vaccines where there is appropriate coordination between researchers, manufacturers and regulators. In any case, such studies should be incorporated into wider research programmes involving larger studies to provide more precise estimates of safety and efficacy (potentially including adaptive trial designs if appropriate). SARS-CoV-2 challenge studies could add value to other types of vaccine research by enabling (a) accurate assessment of asymptomatic infection, (b) more rapid and standardized testing of multiple vaccine candidates, and (c) testing vaccines in contexts where there is little continuing transmission (for example, due to public health measures or during inter-epidemic periods).
Although more data will help to clarify relevant risks, current estimates suggest that participation in SARS-CoV-2 challenge studies would be least risky for young healthy adults. In those aged 18–30 years (whether healthy or not), hospitalization rates for COVID-19 are currently estimated to be around 1% and fatal infection rates around 0.03%. Other long-term health outcomes in this age group are as yet poorly understood. As required by the criteria below, SARS-CoV-2 challenge studies should be conducted in specialized facilities, with especially close monitoring and ready access to early supportive treatment for participants, including critical care if required. However, SARS-CoV-2 challenge studies may (at present) be thought to involve higher levels of risk and uncertainty than other commonly accepted human challenge studies because the pathogenesis of COVID-19 is still poorly understood, the efficacy of the antiviral treatment remdesivir in stopping viral replication still unclear (although it has been shown to shorten hospital stay), and the small but present risk of severe disease or death in young adults. Global public trust in clinical research and vaccines depends on there being heightened vigilance to ensure that, if they proceed, SARS-CoV-2 challenge studies are conducted to the highest scientific and ethical standards. Eight ethical criteria for conducting SARS-CoV-2 challenge studies are set out in Table 2:
Table 2: Eight criteria for SARS-CoV-2 challenge studies
| Criterion 1: SARS-CoV-2 challenge studies must have strong scientific justification. |
| Criterion 2: It must be reasonable to expect that the potential benefits of SARS-CoV-2 challenge studies outweigh risks. |
| Criterion 3: SARS-CoV-2 challenge research programmes should be informed by consultation and engagement with the public as well as relevant experts and policy-makers. |
| Criterion 4: SARS-CoV-2 challenge study research programmes should involve close coordination between researchers, funders, policy-makers and regulators. |
| Criterion 5: SARS-CoV-2 challenge studies should be situated where the research can be conducted to the highest scientific, clinical and ethical standards. |
| Criterion 6: SARS-CoV-2 challenge study researchers should ensure that participant selection criteria limit and minimize risk. |
| Criterion 7: SARS-CoV-2 challenge studies should be reviewed by a specialized independent committee. |
| Criterion 8: SARS-CoV-2 challenge studies must involve rigorous informed consent. |
We remark that it remains the case, to our knowledge, that there is no (statistically significant) evidence that remdesivir reduces the risk of death among COVID-19 patients, though there is some evidence that it shortens recovery time for severely ill patients (by a median of approximately four days), see 182. Since the above W.H.O. report was published, somewhat more effective treatments than remdesivir have been found. In particular, the corticosteroid dexamethasone has been shown (by a large Oxford University study,183 to reduce the death-rate of seriously ill COVID-19 patients on ventilators, by approximately one third; the clinical use of the corticosteroids dexamethasone and hydrocortisone, for patients with severe or critical COVID-19 illness, was subsequently recommended by the W.H.O. on 2nd September, and received MHRA approval on 3rd September. These remain the most effective treatments to have been approved for widespread use. Of course, better treatments may well become available in the near to medium term. As of 1st September, the European Medicines Agency was in discussion with the developers of 158 experimental treatments, including immunomodulators, antivirals and hyperimmune serums.
We give below a summary of the benefits, risks, disadvantages and ethical problems of human challenge trials of candidate vaccines for SARS-CoV-2, and possible ways of mitigating these risks/disadvantages/problems, following the papers and reports cited above.
Benefits
-
Human challenge studies could, through bypassing conventional Phase 3 trials of candidate vaccines, subtract many months from the licensing process, making effective vaccines available much more quickly, and thus reducing the total number of deaths (and cases of severe illness) caused by COVID-19, by many thousands, worldwide.
-
They could enable the rapid and accurate comparison of several candidate vaccines, simultaneously.
Risks, disadvantages, and ethical problems
-
The direct health-risk to volunteers who develop COVID-19 illness (viz., the risk of death or severe illness) as a result of the human challenge trials - in the absence of a highly effective treatment. (We recall that the most effective available treatments, namely corticosteroids, still only reduce the risk of death by approximately one-third.)
-
The infection-risk to third parties (e.g. researchers) during the trials.
-
The risk that public confidence in vaccines may be undermined in the event of untoward effects of challenge studies, possibly reducing public uptake of vaccines in the future.
-
Restricting human challenge trials of a vaccine to young, healthy individuals will not provide information on the level of protection it would give to older/elderly individuals, who are more at risk of severe illness or death, if infected. (Though this disadvantage should be weighed against the fact that vaccines which reduce transmission among younger members of a population, would still have utility in reducing overall transmission.)
-
Human challenge trials are typically small-scale (up to 100 individuals), whereas, to assess potential side-effects of a candidate vaccine, a much larger trial would also be required. (Such a trial, however, would not require any of the individuals involved being exposed to the virus, and would therefore avoid many of the problems of Phase 3 trials.)
Possible measures for mitigating these risks and ethical problems
-
The restriction of human challenge trials to healthy volunteers between the ages of 18 and 30, who are able to give fully-informed consent.
-
Provision of comprehensive information on the risks, to potential volunteers.
-
Continuous monitoring of volunteers, and timely access to state-of-the-art facilities and treatment in the event that they develop Covid-19 illness.
-
Recruiting volunteers from populations who are naturally exposed to a higher level of risk of infection with SARS-CoV-2, than others (e.g., due to living in a country, or working in a sector, experiencing a high infection incidence rate).
-
Protective measures to minimise the risk of infection to third parties.
-
Extensive public consultation before human challenge studies are allowed to commence.
There remain differences of opinion among experts, as to whether human challenge studies of candidate vaccines for SARS-CoV-2 are ethically justified. To cite two high-profile examples, Nir Eyal, Director of Rutgers University’s Centre for Population-Level Bioethics, has argued forcefully in favour,181 whereas Eleanor Riley, formerly Director of the Roslin Institute and Professor of Immunology at Edinburgh University, has argued strongly against.184 These differences of opinion partly hinge on whether the level of risk (of severe illness, or death) to participants is within acceptable limits. Some researchers (such as Eyal, see 181; see also 185) have proposed that risks of organ donation be used for comparison. (It appears that the risk of death to a healthy young adult, when infected with SARS-CoV-2, is similar in magnitude to the risk of dying when donating a kidney.) However, others have pointed out that the equivalence between these scenarios is imperfect, as the benefits of organ donation accrue to an individual close to the donor, whereas the benefits of human challenge trials accrue (in expectation) to the population at large, and furthermore are not guaranteed (as the trial may fail). Some researchers (such as Jamrozik and Selgelid58) have proposed that the background risk (to certain vulnerable populations, e.g. healthcare workers in certain countries) be used for comparison, but (as Jamrozik and Selgelid concede), the objection can be made that high levels of background risk may be caused by injustices or institutional failures (such as a lack of protective equipment).
Questions for further study
Addressing ‘Criterion 2’ in the W.H.O. report, as to whether it is reasonable to expect that the potential benefits of SARS-CoV-2 challenge studies outweigh the risks, would involve making certain assumptions on the likelihood of an effective vaccine being thus developed/accelerated, and the level of protection likely to be provided by such a vaccine to different age-groups, as well as making certain assumptions on how infection incidence will change in different countries, in the medium term. (The latter will, in turn, affect the feasibility, duration and resource requirements of relying solely upon conventional Phase 3 vaccine trials.) Different candidate vaccines are likely to have different risk/benefit trade-offs. For example, the utility of human challenge trials for a candidate vaccine designed to prevent disease (and not transmission), is likely to be less than for others, since the older individuals are much more at risk than younger individuals of poor disease outcomes, immune responses to vaccines can reduce markedly with increasing age, and challenge trials would involve only younger individuals. Nevertheless, we recommend that regulators consider these questions preemptively; amongst other things, this will enable timely implementation of human challenge trials, should Phase 3 trials become infeasible.
To help regulatory authorities to properly address the question of whether human challenge trials of candidate COVID-19 vaccines are ethically justified, we propose the following questions.
-
Given current prevalence estimates (and predictions of medium-term prevalence), what is the feasibility of testing candidate vaccines in conventional Phase 3 trials (both in the UK, and in countries with higher levels of prevalence), and if Phase 3 trials are feasible, how long are they likely to take compared to challenge trials, and what are their resource requirements and potential negative effects?
-
What are the ethical and geopolitical problems of conducting Phase 3 trials in (poorer) countries with high infection-rates, and how can such problems be mitigated, e.g. through compensation?
-
What are the medium-term and long-term effects of moderate illness and severe illness on recovered patients? (This will of course require data from longitudinal studies of patients who suffered moderate and severe illness.)
-
What would be the impact on public support for vaccination programmes, of significant adverse effects on volunteers? (This issue is raised in the extract from the W.H.O. report, above.) Surveys could be designed to help to gauge this.
-
What are the ethically justified ways of reducing the level of risk to each individual volunteer?
-
What are the expected costs of financial compensation for volunteers who suffer long-term effects from exposure? What would be the advantages and disadvantages of promising such compensation explicitly, ahead of the tests? For example, is it likely that it would encourage, or discourage, participation?
-
What would be the costs of insurance against untoward events occurring during the trials? (We note that, even if compensation in the event of long-term effects is not promised ahead of time, it would still be necessary to insure against compensation claims. Moreover, in studies conducted within the NHS/NIHR, participants are entitled to use the NHS complaints processes, so claims could arise irrespective of what compensation, if any, is promised.)
Appendix 2 Vaccines in Development
Vaccines in development as of 3rd September 2020.
For latest updates see: https://vac-lshtm.shinyapps.io/ncov_vaccine_landscape or https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines
| Type of vaccine | In clinical studies | Preclinical studies | Comment | Developers of product in clinical studies |
|---|---|---|---|---|
| Inactivated SARS-CoV-2 virus | 5 | 9 | Need Biosafety Level 3 containment. This is the next to highest level and includes many engineering controls to minimise the chance of escape of the virus. |
Sinovac Wuhan Institute of Biological Products/Sinopharm Beijing Institute of Biological Products/Sinopharm Bharat Biotech Institute of Medical Biology Chinese Academy of Medical Sciences |
| Live attenuated virus | 0 | 3 | Version of the SARS-CoV-2 virus that is modified to be unable to cause disease. | |
| Replicating viral vector | 1 | 17 | Based on several different viruses which contain the gene for a SARS-CoV-2 protein and produce the protein following administration. | Institut Pasteur/Themis/Univ. of Pittsburg CVR/Merck Sharp & Dohme |
| Non replicating viral vector | 6 | 19 | Frequently adenoviral based. The adenovirus contains the gene for a SARS-CoV-2 protein and produces the protein following administration. | University of Oxford/AZ CanSino Biological Inc./Beijing Institute of Biotechnology Gamaleya Research Institute Janssen Pharmaceutical Companies ReiThera/LEUKOCARE/Univercells |
| Virus like particles (VLP) | 1 | 12 | Combination of different components that mimic a virus and generate an immune response. Some baculovirus based | Medicago Inc. |
| Protein subunit | 8 | 50 | Produce individual proteins of the virus biologically. | Novavax Clover Biopharmaceuticals Inc./GSK/Dynavax Anhui Zhifei Longcom Biopharmaceutical/ Institute of Microbiology, Chinese Academy of Sciences Vaxine Pty Ltd/Medytox University of Queensland/GSK/Dynavax Medigen Vaccine Biologics Corporation/NIAID/Dynavax Instituto Finlay de Vacunas, Cuba Kentucky Bioprocessing, Inc University of Queensland/CSL/Seqirus Protein Subunit |
| DNA | 4 | 12 | DNA contains the gene for a SARS-CoV-2 protein and produces the protein following administration. Biologically produced, often needs electroporation to help DNA get into cells. |
Inovio Pharmaceuticals/ International Vaccine Institute Osaka University/ AnGes/ Takara Bio Cadila Healthcare Limited Genexine Consortium |
| RNA | 6 | 16 | RNA contains the gene for a SARS-CoV-2 protein and produces the protein following administration. Chemically synthesised |
Moderna/NIAID BioNTech/Fosun Pharma/Pfizer Imperial College London Curevac People's Liberation Army (PLA) Academy of Military Sciences/Walvax Biotech. Arcturus/Duke-NUS |
Appendix 3 Vaccine production
Production of the ChAdOx1 vaccine
The ChAdOx1 production process starts with preparing the HEK293 cell seed train and the adenovirus inoculum seed train. For this, the HEK293 cells are cultured at increasing volumes until the amounts required for the production bioreactor (commonly at 2000 L working volume) scale are obtained. In the production bioreactor the HEK293 cells are first cultured to reach the required cell densities and then these cells in which the adenovirus can replicate are infected to produce the adenovirus. This adenovirus has been genetically modified to express the SARS-CoV-2 spike protein and it cannot replicate in human cells, thus it is a vector for delivering the genetic material to express the SARS-CoV-2 spike protein. The cell culture and virus production in the bioreactor takes around 7-10 days and it can be operated in fed-batch mode. From the bioreactor, the solution enters the downstream separation and purification section of the process whereby cells are initially lysed then the larger impurities (such as cell debris) are removed using microfiltration where the adenoviral vectors flow through the filter. Next, another particle size-based separation is performed, where the tangential flow ultrafiltration/diafiltration is performed to retain adenoviruses by the filter. Here the adenoviruses are washed, and the buffer is replaced with a buffer suitable for the subsequent ion-exchange chromatography step. In the ion-exchange chromatography step the adenoviral vectors are separated based on electrical charge differences that exist between these adenoviral vectors and other impurities. Following elution from the ion-exchange chromatography, the adenoviral vector solution is sterile filtered, and the buffer can be exchanged for the formulation buffer, using tangential flow ultrafiltration/diafiltration.
Production of self-amplifying RNA vaccines
For saRNA vaccine production the process starts with a cell-free enzymatic reaction, whereby the saRNA molecule is synthesized using the T7 RNA polymerase enzyme based on a DNA template. The saRNA synthesis, (aka. in vitro transcription) reaction takes 2 hours and then the DNA template is digested using the DNAse I enzyme in 15 minutes and then the solution enters the downstream purification section. This reaction mix has a well-defined and simple composition compared to cell-based culture broths, thus the downstream purification is also relatively simple. Downstream purification can consist of tangential flow filtration, whereby the saRNA which is the largest size component is retained by the filter and the other smaller size components flow through the filter. Next, the saRNA can be further purified using CaptoCore 700 multi-modal chromatography. After this the buffer is exchanged for the formulation buffer using tangential flow ultrafiltration/diafiltration. Next, formulation in LNPs takes place, which is the longest duration operation, taking around 9-10 hours to complete. The formulation commonly takes place at the drug substance manufacturing site, to stabilise the RNA molecule. Following formulation, the solution is sterile filtered and can be shipped to the fill-to-finish site.
Overview of Vaccine Manufacturing Processes
| Vaccine type | Manufacturing process | Key features | Selected potential quality issues | Manufacturing issues |
|---|---|---|---|---|
| Inactivated virus | Grow cells, infect cells with virus and then purify and deactivate and potentially add adjuvant | Often needs attachment dependent cell culture Well proven as a vaccine approach |
Removal of host cell material Ensuring inactivation |
Need high biosafety level containment Scalability of attachment dependent cell culture process |
| Attenuated virus | Grow cells, infect cells and then purify and formulate | Often needs attachment dependent cell culture Well proven as a vaccine approach |
Removal of host cell material Contamination with other viruses, mycoplasma and bacteria Ratio of viable to non viable virus need to be optimised |
As the vaccine is not inactivated, there is a possibility that viable contaminants are included in the vaccine. Potential for virus to become infective and start an outbreak. |
| Viral vector (replicating and non replicating) | Cell lines containing viral coding DNA may be used or cells may be infected to produce vaccine | Diverse viruses and cell lines Not established |
Removal of host cell material Contamination with other viruses, mycoplasma and bacteria Ratio of viable to non viable virus need to be optimised |
As the virus is not killed there is a possibility that viable contaminants are included in the vaccine. Many of the viral vectors used are also viruses that will produce strong immune responses. Can they be used repeatedly? |
| Virus like particles | Different methods but baculovirus in insect cells is one approach Engineered mammalian cells offer another approach |
Can be used to present several antigens at once Not established |
Removal of host cell material Contamination with other viruses, mycoplasma and bacteria |
Consistent VLP’s in terms of antigen content |
| Subunit vaccines | Make virus components in cell or microbial culture, purify and formulate, often with adjuvant | Depending on the requirement, glycosylated or non glycosylated product can be made and different proteins can be blended to make the best combination for a vaccine Well established |
Removal of host cell material Glycoform distribution Protein ratios |
Competition for manufacturing capacity with other (therapeutic) proteins |
| DNA vaccines | Grow bacteria containing plasmid DNA, purify, formulate (frequently as a liposome) | Need a good strain of E.coli bacteria that doesn’t recombine the plasmid Not established |
Concatomers Endotoxin Sequence (preventing recombination of plasmid particularly important) Delivery package consistency |
DNA vaccines need to be inside the nucleus of the target cell to work so need protecting and may also need an electroporation device for administration. Storage temperatures may be very low |
| RNA vaccines | Use DNA template to make RNA in a cell free enzymatic reaction, purify, formulate | RNAse free environment must be maintained. Avoiding degradation induced by shear stress Not established |
Sequence Residual reagents Delivery package consistency Sterility |
Formulation to assure delivery inside target cells, prevent degradation and maintain thermostability. Storage temperatures may be very low |
Bibliography
-
Kellam P, Barclay W. The dynamics of humoral immune responses following SARS-CoV-2 infection and the potential for reinfection. J Gen Virol. 2020;101(8):791–7. ↩
-
Yu J, Tostanoski LH, Peter L, Mercado NB, McMahan K, Mahrokhian SH, et al. DNA vaccine protection against SARS-CoV-2 in rhesus macaques. Science. 2020 Aug 14;369(6505):806–11. ↩ ↩2 ↩3
-
Chandrashekar A, Liu J, Martinot AJ, McMahan K, Mercado NB, Peter L, et al. SARS-CoV-2 infection protects against rechallenge in rhesus macaques. Science. 2020 Aug 14;369(6505):812–7. ↩ ↩2 ↩3
-
Pinto D, Park Y-J, Beltramello M, Walls AC, Tortorici MA, Bianchi S, et al. Cross-neutralization of SARS-CoV-2 by a human monoclonal SARS-CoV antibody. Nature. 2020 May 18;583(7815):290–5. ↩
-
Wu Y, Wang F, Shen C, Peng W, Li D, Zhao C, et al. A noncompeting pair of human neutralizing antibodies block COVID-19 virus binding to its receptor ACE2. Science. 2020 Jun 12;368(6496):1274–8. ↩
-
Premkumar L, Segovia-Chumbez B, Jadi R, Martinez DR, Raut R, Markmann A, et al. The receptor binding domain of the viral spike protein is an immunodominant and highly specific target of antibodies in SARS-CoV-2 patients. Sci Immunol. 2020 Jun 11;5(48). ↩
-
Chi X, Yan R, Zhang J, Zhang G, Zhang Y, Hao M, et al. A neutralizing human antibody binds to the N-terminal domain of the Spike protein of SARS-CoV-2. Science. 2020 Aug 7;369(6504):650–5. ↩
-
Brouwer PJM, Caniels TG, van der Straten K, Snitselaar JL, Aldon Y, Bangaru S, et al. Potent neutralizing antibodies from COVID-19 patients define multiple targets of vulnerability. Science. 2020 Aug 7;369(6504):643–50. ↩
-
Weiskopf D, Schmitz KS, Raadsen MP, Grifoni A, Okba NMA, Endeman H, et al. Phenotype and kinetics of SARS-CoV-2-specific T cells in COVID-19 patients with acute respiratory distress syndrome. Sci Immunol. 2020 Jun 26;5(48). ↩ ↩2
-
Grifoni A, Weiskopf D, Ramirez SI, Mateus J, Dan JM, Moderbacher CR, et al. Targets of T Cell Responses to SARS-CoV-2 Coronavirus in Humans with COVID-19 Disease and Unexposed Individuals. Cell. 2020 Jun 25;181(7):1489-1501.e15. ↩ ↩2 ↩3
-
Ni L, Ye F, Cheng M-L, Feng Y, Deng Y-Q, Zhao H, et al. Detection of SARS-CoV-2-Specific Humoral and Cellular Immunity in COVID-19 Convalescent Individuals. Immunity. 2020 Jun 16;52(6):971-977.e3. ↩
-
Peng Y, Mentzer AJ, Liu G, Yao X, Yin Z, Dong D, et al. Broad and strong memory CD4+ and CD8+ T cells induced by SARS-CoV-2 in UK convalescent individuals following COVID-19. Nat Immunol. 2020 Sep 4. ↩ ↩2
-
Sekine T, Perez-Potti A, Rivera-Ballesteros O, Strålin K, Gorin JB, Olsson A, et al. Robust T cell immunity in convalescent individuals with asymptomatic or mild COVID-19. Cell. 2020 Aug 14. ↩ ↩2
-
Gallais F, Velay A, Wendling M-J, Nazon C, Partisani M, Sibilia J, et al. Intrafamilial Exposure to SARS-CoV-2 Induces Cellular Immune Response without Seroconversion. medRxiv. 2020 Jun 22. ↩
-
Cao W-C, Liu W, Zhang P-H, Zhang F, Richardus JH. Disappearance of antibodies to SARS-associated coronavirus after recovery. N Engl J Med. 2007 Sep 13;357(11):1162–3. ↩
-
Ng O-W, Chia A, Tan AT, Jadi RS, Leong HN, Bertoletti A, et al. Memory T cell responses targeting the SARS coronavirus persist up to 11 years post-infection. Vaccine. 2016 Apr 12;34(17):2008–14. ↩
-
Le Bert N, Tan AT, Kunasegaran K, Tham CYL, Hafezi M, Chia A, et al. SARS-CoV-2-specific T cell immunity in cases of COVID-19 and SARS, and uninfected controls. Nature. 2020 Jul 15;584(7821):457–62. ↩ ↩2
-
Sekine T, Perez-Potti A, Rivera-Ballesteros O, Straling K, Gorin J-B, Olsson A, et al. Robust T cell immunity in convalescent individuals with asymptomatic or mild COVID-19. BioRxiv. 2020 Jun 29. ↩
-
Hotez PJ, Corry DB, Strych U, Bottazzi ME. COVID-19 vaccines: neutralizing antibodies and the alum advantage. Nat Rev Immunol. 2020 Jun 4. ↩
-
Iwasaki A, Yang Y. The potential danger of suboptimal antibody responses in COVID-19. Nat Rev Immunol. 2020;20(6):339–41. ↩ ↩2
-
Arvin AM, Fink K, Schmid MA, Cathcart A, Spreafico R, Havenar-Daughton C, et al. A perspective on potential antibody-dependent enhancement of SARS-CoV-2. Nature. 2020 Jul 13;584(7821):353–63. ↩ ↩2
-
Vennema H, de Groot RJ, Harbour DA, Dalderup M, Gruffydd-Jones T, Horzinek MC, et al. Early death after feline infectious peritonitis virus challenge due to recombinant vaccinia virus immunization. J Virol. 1990 Mar;64(3):1407–9. ↩
-
Liu L, Wei Q, Lin Q, Fang J, Wang H, Kwok H, et al. Anti-spike IgG causes severe acute lung injury by skewing macrophage responses during acute SARS-CoV infection. JCI Insight. 2019 Feb 21;4(4). ↩
-
Wan Y, Shang J, Sun S, Tai W, Chen J, Geng Q, et al. Molecular Mechanism for Antibody-Dependent Enhancement of Coronavirus Entry. J Virol. 2020 Feb 14;94(5). ↩
-
Jaume M, Yip MS, Cheung CY, Leung HL, Li PH, Kien F, et al. Anti-severe acute respiratory syndrome coronavirus spike antibodies trigger infection of human immune cells via a pH- and cysteine protease-independent FcγR pathway. J Virol. 2011 Oct 1;85(20):10582–97. ↩
-
Lambert P-H, Ambrosino DM, Andersen SR, Baric RS, Black SB, Chen RT, et al. Consensus summary report for CEPI/BC March 12-13, 2020 meeting: Assessment of risk of disease enhancement with COVID-19 vaccines. Vaccine. 2020 Jun 26;38(31):4783–91. ↩
-
Amanat F, Krammer F. SARS-CoV-2 Vaccines: Status Report. Immunity. 2020 Apr 14;52(4):583–9. ↩
-
COVID-19 vaccine tracker [Internet]. [cited 2020 Sep 12]. Available from: https://vac-lshtm.shinyapps.io/ncov_vaccine_landscape/. ↩
-
Draft landscape of COVID-19 candidate vaccines [Internet]. [cited 2020 Sep 7]. Available from: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines. ↩ ↩2 ↩3 ↩4 ↩5
-
Krammer F. SARS-CoV-2 vaccines in development. Nature. 2020 Sep 23. ↩
-
Zhu F-C, Li Y-H, Guan X-H, Hou L-H, Wang W-J, Li J-X, et al. Safety, tolerability, and immunogenicity of a recombinant adenovirus type-5 vectored COVID-19 vaccine: a dose-escalation, open-label, non-randomised, first-in-human trial. Lancet. 2020 Jun 13;395(10240):1845–54. ↩
-
Folegatti PM, Ewer KJ, Aley PK, Angus B, Becker S, Belij-Rammerstorfer S, et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet. 2020 Aug 15;396(10249):467–78. ↩
-
van Doremalen N, Lambe T, Spencer A, Belij-Rammerstorfer S, Purushotham JN, Port JR, et al. ChAdOx1 nCoV-19 vaccine prevents SARS-CoV-2 pneumonia in rhesus macaques. Nature. 2020 Jul 30. ↩ ↩2 ↩3
-
Graham SP, McLean RK, Spencer AJ, Belij-Rammerstorfer S, Wright D, Ulaszewska M, et al. Evaluation of the immunogenicity of prime-boost vaccination with the replication-deficient viral vectored COVID-19 vaccine candidate ChAdOx1 nCoV-19. npj Vaccines. 2020 Jul 27;5:69. ↩
-
Moderna Announces Positive Interim Phase 1 Data for its mRNA Vaccine (mRNA-1273) Against Novel Coronavirus | Moderna, Inc. [Internet]. [cited 2020 Sep 22]. Available from: https://investors.modernatx.com/news-releases/news-release-details/moderna-announces-positive-interim-phase-1-data-its-mrna-vaccine. ↩
-
Jozwik A, Habibi MS, Paras A, Zhu J, Guvenel A, Dhariwal J, et al. RSV-specific airway resident memory CD8+ T cells and differential disease severity after experimental human infection. Nat Commun. 2015 Dec 21;6:10224. ↩
-
Hervé C, Laupèze B, Del Giudice G, Didierlaurent AM, Tavares Da Silva F. The how’s and what’s of vaccine reactogenicity. npj Vaccines. 2019 Sep 24;4:39. ↩ ↩2 ↩3
-
Plotkin SA. Correlates of protection induced by vaccination. Clin Vaccine Immunol. 2010 Jul;17(7):1055–65. ↩ ↩2
-
Plotkin SA, Gilbert PB. Nomenclature for immune correlates of protection after vaccination. Clin Infect Dis. 2012 Jun;54(11):1615–7. ↩
-
Development and Licensure of Vaccines to Prevent COVID-19 | FDA [Internet]. [cited 2020 Sep 12]. Available from: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/development-and-licensure-vaccines-prevent-covid-19. ↩ ↩2 ↩3
-
WHO Working Group on the Clinical Characterisation and Management of COVID-19 infection. A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect Dis. 2020 Jun 12;20(8):e192–7. ↩ ↩2
-
Chastain DB, Osae SP, Henao-Martínez AF, Franco-Paredes C, Chastain JS, Young HN. Racial disproportionality in covid clinical trials. N Engl J Med. 2020 Aug 11. ↩
-
Alexander PE, Debono VB, Mammen MJ, Iorio A, Aryal K, Deng D, et al. COVID-19 coronavirus research has overall low methodological quality thus far: case in point for chloroquine/hydroxychloroquine. J Clin Epidemiol. 2020 Apr 21. ↩
-
“We are not guinea pigs,” say South African anti-vaccine protesters | Reuters [Internet]. [cited 2020 Sep 24]. Available from: https://uk.reuters.com/article/uk-health-coronavirus-safrica-vaccine/we-are-not-guinea-pigs-say-south-african-anti-vaccine-protesters-idUKKBN2426SA. ↩
-
Lakdawala SS, Menachery VD. The search for a COVID-19 animal model. Science. 2020 May 29;368(6494):942–3. ↩ ↩2
-
Wang H, Zhang Y, Huang B, Deng W, Quan Y, Wang W, et al. Development of an Inactivated Vaccine Candidate, BBIBP-CorV, with Potent Protection against SARS-CoV-2. Cell. 2020 Aug 6;182(3):713-721.e9. ↩
-
Deng W, Bao L, Liu J, Xiao C, Liu J, Xue J, et al. Primary exposure to SARS-CoV-2 protects against reinfection in rhesus macaques. Science. 2020 Aug 14;369(6505):818–23. ↩
-
Shi J, Wen Z, Zhong G, Yang H, Wang C, Huang B, et al. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS-coronavirus 2. Science. 2020 May 29;368(6494):1016–20. ↩
-
Ryan KA, Bewley KR, Fotheringham SA, Brown P, Hall Y, Marriott AC, et al. Dose-dependent response to infection with SARS-CoV-2 in the ferret model: evidence of protection to re-challenge. BioRxiv. 2020 May 29. ↩ ↩2
-
Hassan AO, Case JB, Winkler ES, Thackray LB, Kafai NM, Bailey AL, et al. A SARS-CoV-2 Infection Model in Mice Demonstrates Protection by Neutralizing Antibodies. Cell. 2020 Aug 6;182(3):744-753.e4. ↩
-
Israelow B, Song E, Mao T, Lu P, Meir A, Liu F, et al. Mouse model of SARS-CoV-2 reveals inflammatory role of type I interferon signaling. J Exp Med. 2020 Dec 7;217(12). ↩ ↩2
-
Dinnon KH, Leist SR, Schäfer A, Edwards CE, Martinez DR, Montgomery SA, et al. A mouse-adapted model of SARS-CoV-2 to test COVID-19 countermeasures. Nature. 2020 Aug 27. ↩
-
Winkler ES, Bailey AL, Kafai NM, Nair S, McCune BT, Yu J, et al. SARS-CoV-2 infection of human ACE2-transgenic mice causes severe lung inflammation and impaired function. Nat Immunol. 2020 Aug 24. ↩
-
Rogers TF, Zhao F, Huang D, Beutler N, Burns A, He W-T, et al. Isolation of potent SARS-CoV-2 neutralizing antibodies and protection from disease in a small animal model. Science. 2020 Aug 21;369(6506):956–63. ↩
-
Gao Q, Bao L, Mao H, Wang L, Xu K, Yang M, et al. Rapid development of an inactivated vaccine candidate for SARS-CoV-2. Science. 2020 May 6. ↩
-
Erasmus JH, Khandhar AP, O’Connor MA, Walls AC, Hemann EA, Murapa P, et al. An Alphavirus-derived replicon RNA vaccine induces SARS-CoV-2 neutralizing antibody and T cell responses in mice and nonhuman primates. Sci Transl Med. 2020 Aug 5;12(555). ↩
-
Eyal N, Lipsitch M, Smith PG. Human challenge studies to accelerate coronavirus vaccine licensure. J Infect Dis. 2020 May 11;221(11):1752–6. ↩ ↩2
-
Jamrozik E, Selgelid MJ. COVID-19 human challenge studies: ethical issues. Lancet Infect Dis. 2020 May 29. ↩ ↩2 ↩3
-
WHO | Key criteria for the ethical acceptability of COVID-19 human challenge studies [Internet]. [cited 2020 Jun 11]. Available from: https://www.who.int/ethics/publications/key-criteria-ethical-acceptability-of-covid-19-human-challenge/en/. ↩
-
Carfì A, Bernabei R, Landi F, Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA. 2020 Jul 9. ↩
-
Demicheli V, Jefferson T, Ferroni E, Rivetti A, Di Pietrantonj C. Vaccines for preventing influenza in healthy adults. Cochrane Database Syst Rev. 2018 Feb 1;2:CD001269. ↩
-
Accelerating a safe and effective COVID-19 vaccine [Internet]. [cited 2020 Aug 19]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov/accelerating-a-safe-and-effective-covid-19-vaccine. ↩ ↩2 ↩3
-
Saad-Roy CM, Wagner CE, Baker RE, Morris SE, Farrar J, Graham AL, et al. Immuno-epidemiological life-history and the dynamics of SARS-CoV-2 over the next five years. medRxiv. 2020 Jul 16. ↩ ↩2 ↩3 ↩4 ↩5 ↩6 ↩7
-
Information R. WHO Strategic Advisory Group of Experts (SAGE) on Immunization Working Group on COVID-19 Vaccines: Prioritized Infectious Disease and Economic Modelling Questions. ↩ ↩2
-
Matrajt L, Eaton J, Leung T, Brown ER. Vaccine optimization for COVID-19, who to vaccinate first? medRxiv. 2020 Aug 15. ↩ ↩2 ↩3 ↩4 ↩5
-
Knight SR, Ho A, Pius R, Buchan I, Carson G, Drake TM, et al. Risk stratification of patients admitted to hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score. BMJ. 2020 Sep 9;370:m3339. ↩
-
Dahlke C, Heidepriem J, Kobbe R, Santer R, Koch T, Fathi A, et al. Distinct early IgA profile may determine severity of COVID-19 symptoms: an immunological case series. medRxiv. 2020 Apr 17. ↩
-
World Economic Outlook, April 2020: The Great Lockdown [Internet]. [cited 2020 Aug 25]. Available from: https://www.imf.org/en/Publications/WEO/Issues/2020/04/14/weo-april-2020. ↩
-
Pronker ES, Weenen TC, Commandeur H, Claassen EHJHM, Osterhaus ADME. Risk in vaccine research and development quantified. PLoS ONE. 2013 Mar 20;8(3):e57755. ↩ ↩2
-
Pronker ES, Weenen TC, Commandeur HR, Osterhaus ADME, Claassen HJHM. The gold industry standard for risk and cost of drug and vaccine development revisited. Vaccine. 2011 Aug 11;29(35):5846–9. ↩
-
Gouglas D, Thanh Le T, Henderson K, Kaloudis A, Danielsen T, Hammersland NC, et al. Estimating the cost of vaccine development against epidemic infectious diseases: a cost minimisation study. Lancet Glob Health. 2018 Oct 18;6(12):e1386–96. ↩
-
Snyder CM, Hoyt K, Gouglas D, Johnston T, Robinson J. Designing Pull Funding For A COVID-19 Vaccine. Health Aff (Millwood). 2020 Jul 23;101377hlthaff202000646. ↩ ↩2 ↩3
-
OECD. Treatments and a vaccine for COVID-19: the need for coordinating policies on R&D, manufacturing and access. OECD; 2020 May. ↩ ↩2
-
Kremer M, Levin J, Snyder C. Advance Market Commitments: Insights from Theory and Experience. Cambridge, MA: National Bureau of Economic Research; 2020 Feb. ↩ ↩2 ↩3 ↩4
-
Morel CM, Mossialos E. Stoking the antibiotic pipeline. BMJ. 2010 May 18;340:c2115. ↩
-
Berndt ER, Glennerster R, Kremer MR, Lee J, Levine R, Weizsäcker G, et al. Advance market commitments for vaccines against neglected diseases: estimating costs and effectiveness. Health Econ. 2007 May;16(5):491–511. ↩ ↩2 ↩3
-
Light DW. Saving the pneumococcal AMC and GAVI. Hum Vaccin. 2011 Feb;7(2):138–41. ↩
-
April 2020 NBER Digest [Internet]. [cited 2020 Aug 12]. Available from: https://nber.org/digest/apr20/w26775.shtml. ↩
-
Usher AD. COVID-19 vaccines for all? Lancet. 2020 Jun 13;395(10240):1822–3. ↩ ↩2 ↩3 ↩4
-
Over £100 million cash boost to manufacture millions of doses of COVID-19 vaccine - GOV.UK [Internet]. [cited 2020 Sep 12]. Available from: https://www.gov.uk/government/news/over-100-million-cash-boost-to-manufacture-millions-of-doses-of-covid-19-vaccine. ↩
-
Callaway E. The unequal scramble for coronavirus vaccines - by the numbers. Nature. 2020;584(7822):506–7. ↩ ↩2
-
UK government invests in Livingston facility to bolster vaccine manufacturing capacity - GOV.UK [Internet]. [cited 2020 Aug 12]. Available from: https://www.gov.uk/government/news/uk-government-invests-in-livingston-facility-to-bolster-vaccine-manufacturing-capacity. ↩
-
Jab economics - Hard questions as scientists and governments seek covid-19 vaccines | Finance & economics | The Economist [Internet]. [cited 2020 Aug 12]. Available from: https://www.economist.com/finance-and-economics/2020/08/08/hard-questions-as-scientists-and-governments-seek-covid-19-vaccines. ↩
-
BD Receives Order from U.K. Government for 65 Million Injection Devices to Support COVID-19 Vaccination Campaign [Internet]. [cited 2020 Aug 12]. Available from: https://www.bd.com/en-uk/about-bd/news-and-media/press-releases/bd-receives-order-from-uk-government-for-65-million-injection-devices-to-support-covid-19-vaccination-campaign. ↩
-
Slaoui M, Hepburn M. Developing Safe and Effective Covid Vaccines - Operation Warp Speed’s Strategy and Approach. N Engl J Med. 2020 Aug 26. ↩
-
Yamey G, Schäferhoff M, Hatchett R, Pate M, Zhao F, McDade KK. Ensuring global access to COVID-19 vaccines. Lancet. 2020 May 2;395(10234):1405–6. ↩
-
Opinion | In the Race for a Coronavirus Vaccine, We Must Go Big. Really, Really Big. - The New York Times [Internet]. [cited 2020 Aug 25]. Available from: https://www.nytimes.com/2020/05/04/opinion/coronavirus-vaccine.html. ↩
-
COVAX explained | Gavi, the Vaccine Alliance [Internet]. [cited 2020 Sep 12]. Available from: https://www.gavi.org/vaccineswork/covax-explained. ↩
-
COVAX: Working for global equitable access to COVID-19 vaccines [Internet]. [cited 2020 Sep 12]. Available from: https://www.who.int/initiatives/act-accelerator/covax. ↩ ↩2
-
Exclusive: Vaccine group says 76 rich countries now committed to “COVAX” access plan | Reuters [Internet]. [cited 2020 Sep 12]. Available from: https://www.reuters.com/article/us-health-coronavirus-vaccines-covax-exc-idUSKBN25T39P. ↩
-
Chinazzi M, Davis J, Dean N, Mu K, Piontti A, Xiong X, et al. Estimating the effect of cooperative versus uncooperative strategies of COVID-19 vaccine allocation: a modeling study. ↩ ↩2
-
CEPI survey assesses potential COVID-19 vaccine manufacturing capacity – CEPI [Internet]. [cited 2020 Sep 13]. Available from: https://cepi.net/news_cepi/cepi-survey-assesses-potential-covid-19-vaccine-manufacturing-capacity/. ↩
-
Khamsi R. If a coronavirus vaccine arrives, can the world make enough? Nature. 2020;580(7805):578–80. ↩ ↩2 ↩3
-
Smith J, Lipsitch M, Almond JW. Vaccine production, distribution, access, and uptake. Lancet. 2011 Jul 30;378(9789):428–38. ↩ ↩2
-
UK government secures new COVID-19 vaccines and backs global clinical trial - GOV.UK [Internet]. [cited 2020 Sep 7]. Available from: https://www.gov.uk/government/news/uk-government-secures-new-covid-19-vaccines-and-backs-global-clinical-trial. ↩ ↩2
-
Oxford’s Covid-19 Vaccine Is the Coronavirus Front-Runner - Bloomberg [Internet]. [cited 2020 Sep 7]. Available from: https://www.bloomberg.com/news/features/2020-07-15/oxford-s-covid-19-vaccine-is-the-coronavirus-front-runner. ↩
-
Coronavirus Vaccine: AstraZeneca (AZN) Seeks Doses by September - Bloomberg [Internet]. [cited 2020 Sep 7]. Available from: https://www.bloomberg.com/news/articles/2020-05-17/astrazeneca-aims-for-30-million-u-k-vaccine-doses-by-september. ↩
-
Britain Secures 90 Million Doses Of Potential Coronavirus Vaccines From Pfizer, BioNTech & Valneva [Internet]. [cited 2020 Sep 7]. Available from: https://www.forbes.com/sites/isabeltogoh/2020/07/20/britain-secures-90-million-doses-of-potential-coronavirus-vaccines-from-pfizer-biontech--valneva/\#be3d8254ae2e. ↩
-
Pfizer and BioNTech Announce Agreement with the United Kingdom for 30 Million Doses of mRNA-based Vaccine Candidate against SARS-CoV-2 | Pfizer [Internet]. [cited 2020 Sep 7]. Available from: https://www.pfizer.com/news/press-release/press-release-detail/pfizer-and-biontech-announce-agreement-united-kingdom-30. ↩
-
Pfizer and BioNTech Dose First Participants in the U.S. as Part of Global COVID-19 mRNA Vaccine Development Program | Pfizer [Internet]. [cited 2020 Sep 7]. Available from: https://www.pfizer.com/news/press-release/press-release-detail/pfizer_and_biontech_dose_first_participants_in_the_u_s_as_part_of_global_covid_19_mrna_vaccine_development_program. ↩
-
Biological E to manufacture Janssen’s Covid-19 vaccine [Internet]. [cited 2020 Sep 7]. Available from: https://www.pharmaceutical-technology.com/news/biological-e-covid-vaccine-deals/. ↩
-
Novavax and UK Government Announce Collaboration and Purchase Agreement for Novavax’ COVID-19 Vaccine Candidate | Novavax Inc. - IR Site [Internet]. [cited 2020 Sep 7]. Available from: https://ir.novavax.com/news-releases/news-release-details/novavax-and-uk-government-announce-collaboration-and-purchase. ↩
-
U.K. Government-Backed Centre for Process Innovation (CPI) Scaling Up Imperial’s Coronavirus Vaccine [Internet]. [cited 2020 Sep 7]. Available from: https://www.genengnews.com/topics/bioprocessing/u-k-government-backed-centre-for-process-innovation-cpi-scaling-up-imperials-coronavirus-vaccine/. ↩
-
Valneva Confirms Participation in UK Government COVID-19 Vaccine Response Program – Valneva [Internet]. [cited 2020 Sep 7]. Available from: https://valneva.com/press-release/valneva-confirms-participation-in-uk-government-covid-19-vaccine-response-program/. ↩
-
Sanofi and GSK agree with the UK government to supply up to 60 million doses of COVID-19 vaccine | GSK [Internet]. [cited 2020 Sep 7]. Available from: https://www.gsk.com/en-gb/media/press-releases/sanofi-and-gsk-agree-with-the-uk-government-to-supply-up-to-60-million-doses-of-covid-19-vaccine/. ↩
-
Sanofi and GSK selected for Operation Warp Speed to supply United States Government with 100 million doses of COVID-19 vaccine | GSK [Internet]. [cited 2020 Sep 7]. Available from: https://www.gsk.com/en-gb/media/press-releases/sanofi-and-gsk-selected-for-operation-warp-speed-to-supply-united-states-government-with-100-million-doses-of-covid-19-vaccine/. ↩
-
IATA - The Time to Prepare for COVID-19 Vaccine Transport is Now [Internet]. [cited 2020 Sep 10]. Available from: https://www.iata.org/en/pressroom/pr/2020-09-09-01/. ↩ ↩2
-
Coronavirus: Health workers’ army to be trained to deliver Covid vaccine - BBC News [Internet]. [cited 2020 Sep 7]. Available from: https://www.bbc.co.uk/news/health-53946412. ↩
-
RAPID ASSISTANCE IN MODELLING THE PANDEMIC: RAMP [Internet]. [cited 2020 Sep 7]. Available from: https://epcced.github.io/ramp/. ↩
-
Nuffield Council on Bioethics. Fair and equitable access to COVID-19 treatments and vaccines [Internet]. Policy briefing: Key challenges for ensuring fair and equitable access to COVID-19 vaccines and treatments. 2020 [cited 2020 Sep 29]. Available from: https://www.nuffieldbioethics.org/news/policy-briefing-key-challenges-for-ensuring-fair-and-equitable-access-to-covid-19-vaccines-and-treatments. ↩
-
Daniels N. Accountability for reasonableness. BMJ. 2000 Nov 25;321(7272):1300–1. ↩
-
Cookson R, Mirelman AJ, Griffin S, Asaria M, Dawkins B, Norheim OF, et al. Using Cost-Effectiveness Analysis to Address Health Equity Concerns. Value Health. 2017;20(2):206–12. ↩
-
How might COVID-19 affect the number of GPs available to see patients in England? | The Health Foundation [Internet]. [cited 2020 Sep 12]. Available from: https://www.health.org.uk/publications/long-reads/how-might-covid-19-affect-the-number-of-gps-available-to-see-patients-in-england. ↩
-
Smith RD, Correa C, Oh C. Trade, TRIPS, and pharmaceuticals. Lancet. 2009 Feb 21;373(9664):684–91. ↩
-
Hoen E ’t, Berger J, Calmy A, Moon S. Driving a decade of change: HIV/AIDS, patents and access to medicines for all. J Int AIDS Soc. 2011 Mar 27;14:15. ↩
-
The rush to create a covid-19 vaccine may do more harm than good - The BMJ [Internet]. [cited 2020 Aug 10]. Available from: https://blogs.bmj.com/bmj/2020/08/05/the-rush-to-create-a-covid-19-vaccine-may-do-more-harm-than-good/. ↩
-
Jiang S. Don’t rush to deploy COVID-19 vaccines and drugs without sufficient safety guarantees. Nature. 2020;579(7799):321. ↩
-
Krause P, Fleming TR, Longini I, Henao-Restrepo AM, Peto R, World Health Organization Solidarity Vaccines Trial Expert Group. COVID-19 vaccine trials should seek worthwhile efficacy. Lancet. 2020 Aug 27. ↩ ↩2 ↩3 ↩4
-
Harrison EA, Wu JW. Vaccine confidence in the time of COVID-19. Eur J Epidemiol. 2020 Apr 22;35(4):325–30. ↩
-
Gellin B. Why vaccine rumours stick—and getting them unstuck. Lancet. 2020 Aug;396(10247):303–4. ↩
-
Van Bavel JJ, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M, et al. Using Social and Behavioural Science to Support COVID-19 Pandemic Response. Nat Hum Behav. 2020 Apr 30;4(5):460–71. ↩
-
Schmid P, Betsch C. Effective strategies for rebutting science denialism in public discussions. Nat Hum Behav. 2019 Jun 24;3(9):931–9. ↩
-
Bholat D, Broughton N, Ter Meer J, Walczak E. Enhancing central bank communications using simple and relatable information. J Monet Econ. 2019 Dec;108:1–15. ↩
-
Haldane A, McMahon M. Central bank communications and the general public. AEA Papers and Proceedings. 2018 May 1;108:578–83. ↩
-
Haldane A, Macaulay A, McMahon M. The 3 E’s of Central Bank Communication with the Public. SSRN Journal. 2020. ↩
-
Haydarov R, Anand S, Frouws B, Toure B, Okiror S, Bhui BR. Evidence-Based Engagement of the Somali Pastoralists of the Horn of Africa in Polio Immunization: Overview of Tracking, Cross-Border, Operations, and Communication Strategies. Global Health Communication. 2016 Jan;2(1):11–8. ↩
-
Schuster M, Duclos P. WHO Recommendations Regarding Vaccine Hesitancy. Vaccine. 2015 Aug 14;33(34):4155–218. ↩
-
Jarrett C, Wilson R, O’Leary M, Eckersberger E, Larson HJ, SAGE Working Group on Vaccine Hesitancy. Strategies for addressing vaccine hesitancy - A systematic review. Vaccine. 2015 Aug 14;33(34):4180–90. ↩ ↩2
-
Peretti-Watel P, Larson HJ, Ward JK, Schulz WS, Verger P. Vaccine hesitancy: clarifying a theoretical framework for an ambiguous notion. PLoS Curr Influenza. 2015 Feb 25;7. ↩
-
Lyons BA, Hasell A, Tallapragada M, Jamieson KH. Conversion messages and attitude change: Strong arguments, not costly signals. Public Underst Sci. 2019 Jan 10;28(3):320–38. ↩
-
Levine JM, Valle RS. The convert as a credible communicator. Soc Behav Pers. 1975 Jan 1;3(1):81–90. ↩
-
Harris K, Maurer J, Black C, Euler G, Kadiyala S. Workplace efforts to promote influenza vaccination among healthcare personnel and their association with uptake during the 2009 pandemic influenza A (H1N1). Vaccine. 2011 Apr 5;29(16):2978–85. ↩
-
Cover of vaccination evaluated rapidly (COVER) programme 2014 to 2015: quarterly data - GOV.UK [Internet]. [cited 2020 Aug 6]. Available from: https://www.gov.uk/government/statistics/cover-of-vaccination-evaluated-rapidly-cover-programme-2014-to-2015-quarterly-data. ↩
-
Forster AS, Rockliffe L, Chorley AJ, Marlow LAV, Bedford H, Smith SG, et al. Ethnicity-specific factors influencing childhood immunisation decisions among Black and Asian Minority Ethnic groups in the UK: a systematic review of qualitative research. J Epidemiol Community Health. 2017;71(6):544–9. ↩ ↩2
-
Martin KD, Roter DL, Beach MC, Carson KA, Cooper LA. Physician communication behaviors and trust among black and white patients with hypertension. Med Care. 2013 Feb;51(2):151–7. ↩
-
Brooks LA, Manias E, Bloomer MJ. Culturally sensitive communication in healthcare: A concept analysis. Collegian. 2018 Oct. ↩
-
Cohen J. The line is forming for a COVID-19 vaccine. Who should be at the front? Science. 2020 Jun 29. ↩ ↩2 ↩3 ↩4
-
Awasthi R, Guliani KK, Bhatt A, Gill MS, Nagori A, Kumaraguru P, et al. VacSIM: Learning Effective Strategies for COVID-19 Vaccine Distribution using Reinforcement Learning. arXiv. 2020 Sep 14. ↩ ↩2
-
Britton T, Ball F, Trapman P. A mathematical model reveals the influence of population heterogeneity on herd immunity to SARS-CoV-2. Science. 2020 Jun 23. ↩ ↩2 ↩3
-
Bubar KM, Kissler SM, Lipsitch M, Cobey S, Grad Y, Larremore DB. Model-informed COVID-19 vaccine prioritization strategies by age and serostatus. medRxiv. 2020 Sep 10. ↩ ↩2 ↩3
-
Coronavirus and shielding of clinically extremely vulnerable people in England - Office for National Statistics [Internet]. [cited 2020 Sep 15]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/coronavirusandshieldingofclinicallyextremelyvulnerablepeopleinengland/9julyto16july2020\#main-points. ↩ ↩2
-
Old age structure variant - UK population in age groups - Office for National Statistics [Internet]. [cited 2020 Sep 15]. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/datasets/tablel21oldagestructurevariantukpopulationinagegroups. ↩
-
Report 33 - Modelling the allocation and impact of a COVID-19 vaccine | Faculty of Medicine | Imperial College London [Internet]. [cited 2020 Sep 25]. Available from: https://www.imperial.ac.uk/mrc-global-infectious-disease-analysis/covid-19/report-33-vaccine/. ↩ ↩2 ↩3
-
Joint Committee on Vaccination and Immunisation: interim advice on priority groups for COVID-19 vaccination - GOV.UK [Internet]. [cited 2020 Aug 3]. Available from: https://www.gov.uk/government/publications/priority-groups-for-coronavirus-covid-19-vaccination-advice-from-the-jcvi/interim-advice-on-priority-groups-for-covid-19-vaccination. ↩ ↩2
-
Key workers reference tables - Office for National Statistics [Internet]. [cited 2020 Sep 15]. Available from: https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/earningsandworkinghours/datasets/keyworkersreferencetables. ↩
-
Karafillakis E, Dinca I, Apfel F, Cecconi S, Wűrz A, Takacs J, et al. Vaccine hesitancy among healthcare workers in Europe: A qualitative study. Vaccine. 2016 Sep 22;34(41):5013–20. ↩
-
The DELVE Initiative. Scoping Report on Hospital and Health Care Acquisition of COVID-19 and its Control. [Internet]. 2020 [cited 2020 Sep 24]. Available from: https://rs-delve.github.io/reports/2020/07/06/nosocomial-scoping-report.html. ↩
-
Hayward AC, Harling R, Wetten S, Johnson AM, Munro S, Smedley J, et al. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ. 2006 Dec 16;333(7581):1241. ↩
-
Baguelin M, Flasche S, Camacho A, Demiris N, Miller E, Edmunds WJ. Assessing optimal target populations for influenza vaccination programmes: an evidence synthesis and modelling study. PLoS Med. 2013 Oct 8;10(10):e1001527. ↩
-
Carman WF, Elder AG, Wallace LA, McAulay K, Walker A, Murray GD, et al. Effects of influenza vaccination of health-care workers on mortality of elderly people in long-term care: a randomised controlled trial. Lancet. 2000 Jan 8;355(9198):93–7. ↩
-
Davies NG, Klepac P, Liu Y, Prem K, Jit M, CMMID COVID-19 working group, et al. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med. 2020 Jun 16;26(8):1205–11. ↩
-
Viner RM, Mytton OT, Bonell C, Melendez-Torres GJ, Ward JL, Hudson L, et al. Susceptibility to and transmission of COVID-19 amongst children and adolescents compared with adults: a systematic review and meta-analysis. medRxiv. 2020 May 24. ↩
-
Fontanet A, Cauchemez S. COVID-19 herd immunity: where are we? Nat Rev Immunol. 2020 Oct;20(10):583–4. ↩
-
Flaxman S, Mishra S, Gandy A, Unwin H, Coupland H, Mellan T, et al. Report 13: Estimating the number of infections and the impact of non-pharmaceutical interventions on COVID-19 in 11 European countries. Imperial College London. 2020. ↩
-
Randolph HE, Barreiro LB. Herd Immunity: Understanding COVID-19. Immunity. 2020 May 19;52(5):737–41. ↩
-
Scherer A, McLean A. Mathematical models of vaccination. Br Med Bull. 2002;62:187–99. ↩ ↩2
-
Béraud G. Mathematical models and vaccination strategies. Vaccine. 2018 Aug 28;36(36):5366–72. ↩
-
Hepatitis A: the green book, chapter 17 - GOV.UK [Internet]. [cited 2020 Sep 24]. Available from: https://www.gov.uk/government/publications/hepatitis-a-the-green-book-chapter-17. ↩
-
Lurie N, Sharfstein JM, Goodman JL. The Development of COVID-19 Vaccines: Safeguards Needed. JAMA. 2020 Aug 4;324(5):439–40. ↩
-
Sanjuán R, Nebot MR, Chirico N, Mansky LM, Belshaw R. Viral mutation rates. J Virol. 2010 Oct;84(19):9733–48. ↩
-
Bar-On YM, Flamholz A, Phillips R, Milo R. SARS-CoV-2 (COVID-19) by the numbers. elife. 2020 Apr 2;9. ↩
-
SET-C. The SARS-CoV-2 genome: variation, implication and application. The Royal Society; 2020 Aug. ↩ ↩2
-
Vijgen L, Keyaerts E, Lemey P, Moës E, Li S, Vandamme A-M, et al. Circulation of genetically distinct contemporary human coronavirus OC43 strains. Virology. 2005 Jun 20;337(1):85–92. ↩
-
Ren L, Zhang Y, Li J, Xiao Y, Zhang J, Wang Y, et al. Genetic drift of human coronavirus OC43 spike gene during adaptive evolution. Sci Rep. 2015 Jun 22;5:11451. ↩
-
Weisblum Y, Schmidt F, Zhang F, DaSilva J, Poston D, Lorenzi JCC, et al. Escape from neutralizing antibodies by SARS-CoV-2 spike protein variants. BioRxiv. 2020 Jul 22. ↩
-
Moderna pitches virus vaccine at about $50-$60 per course | Financial Times [Internet]. [cited 2020 Sep 24]. Available from: https://www.ft.com/content/405c0d07-d15a-4f5b-8a77-3c2fbd5d4c1c. ↩
-
Gouglas D, Christodoulou M, Plotkin SA, Hatchett R. CEPI: driving progress toward epidemic preparedness and response. Epidemiol Rev. 2019 Jan 31;41(1):28–33. ↩
-
Plotkin SA. Vaccines for epidemic infections and the role of CEPI. Hum Vaccin Immunother. 2017 Dec 2;13(12):2755–62. ↩
-
Røttingen J-A, Gouglas D, Feinberg M, Plotkin S, Raghavan KV, Witty A, et al. New Vaccines against Epidemic Infectious Diseases. N Engl J Med. 2017 Feb 16;376(7):610–3. ↩
-
Moon S, Sridhar D, Pate MA, Jha AK, Clinton C, Delaunay S, et al. Will Ebola change the game? Ten essential reforms before the next pandemic. The report of the Harvard-LSHTM Independent Panel on the Global Response to Ebola. Lancet. 2015 Nov 28;386(10009):2204–21. ↩
-
Currie J, Grenfell B, Farrar J. Infectious diseases. Beyond Ebola. Science. 2016 Feb 19;351(6275):815–6. ↩ ↩2
-
Kis Z, Kontoravdi C, Dey AK, Shattock R, Shah N. Rapid development and deployment of high‐volume vaccines for pandemic response. Jnl Adv Manuf & Process. 2020 Jul;2(3). ↩
-
Bloom DE, Black S, Rappuoli R. Emerging infectious diseases: A proactive approach. Proc Natl Acad Sci USA. 2017 Apr 18;114(16):4055–9. ↩
-
Graham BS, Sullivan NJ. Emerging viral diseases from a vaccinology perspective: preparing for the next pandemic. Nat Immunol. 2018 Jan;19(1):20–8. ↩
-
Osterholm M, Moore K, Ostrowsky J, Kimball-Baker K, Farrar J, Wellcome Trust-CIDRAP Ebola Vaccine Team B. The Ebola Vaccine Team B: a model for promoting the rapid development of medical countermeasures for emerging infectious disease threats. Lancet Infect Dis. 2016 Jan;16(1):e1–9. ↩
-
Rappuoli R, Hanon E. Sustainable vaccine development: a vaccine manufacturer’s perspective. Curr Opin Immunol. 2018 May 8;53:111–8. ↩
-
Hoyt K, Hatchett R. Preparing for the next Zika. Nat Biotechnol. 2016 Apr;34(4):384–6. ↩
-
Plotkin SA. Vaccines we need but don’t have. Viral Immunol. 2018;31(2):114–6. ↩
-
Poland GA, Whitaker JA, Poland CM, Ovsyannikova IG, Kennedy RB. Vaccinology in the third millennium: scientific and social challenges. Curr Opin Virol. 2016 Mar 30;17:116–25. ↩
-
Sheerin D, Openshaw PJ, Pollard AJ. Issues in vaccinology: Present challenges and future directions. Eur J Immunol. 2017 Sep 27;47(12):2017–25. ↩
-
WHO conditionally backs Covid-19 vaccine trials that infect people | Science | The Guardian [Internet]. [cited 2020 Sep 15]. Available from: https://www.theguardian.com/science/2020/may/08/who-conditionally-backs-covid-19-vaccine-trials-that-infect-people. ↩ ↩2 ↩3
-
Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, et al. Remdesivir for the Treatment of Covid-19 - Preliminary Report. N Engl J Med. 2020 May 22. ↩
-
RECOVERY Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in Hospitalized Patients with Covid-19 - Preliminary Report. N Engl J Med. 2020 Jul 17. ↩
-
UK scientists want to infect volunteers with Covid-19 in race to find vaccine | Society | The Guardian [Internet]. [cited 2020 Sep 15]. Available from: https://www.theguardian.com/society/2020/may/24/uk-scientists-want-to-infect-volunteers-with-covid-19-in-race-to-find-vaccine. ↩
-
Miller FG, Joffe S. Limits to research risks. J Med Ethics. 2009 Jul;35(7):445–9. ↩