[edit]
Face Masks for the General Public
An update to this report is now available here.
An earlier version of this document was communicated to SAGE in April 2020.
Summary
Face masks could offer an important tool for contributing to the management of community transmission of Covid19 within the general population. Evidence supporting their potential effectiveness comes from analysis of: (1) the incidence of asymptomatic and pre-symptomatic transmission; (2) the role of respiratory droplets in transmission, which can travel as far as 1-2 meters; and (3) studies of the use of homemade and surgical masks to reduce droplet spread. Our analysis suggests that their use could reduce onward transmission by asymptomatic and pre-symptomatic wearers if widely used in situations where physical distancing is not possible or predictable, contrasting to the standard use of masks for the protection of wearers. If correctly used on this basis, face masks, including homemade cloth masks, can contribute to reducing viral transmission.
Citation
(2020), Face Masks for the General Public. DELVE Report No. 1. Published 04 May 2020. Available from https://rs-delve.github.io/reports/2020/05/04/face-masks-for-the-general-public.html [pdf].
Table of Contents
- Key Points
- Policy Implications
- Areas where further investigation is needed
- Evidence Base
- Appendix: Mask policies in different countries
- Additional Material
- Footnotes and References
Key points
-
Asymptomatic (including presymptomatic) infected individuals are infectious. Without mitigation, the current estimate is that 40%-80% of infections occur from individuals without symptoms1 2 3 4. Universal screening of asymptomatic SARS-COV2 in women admitted for delivery in New York City shows that 13.7% were infected, and that asymptomatic women accounted for 88% of infected individuals in the study5. Of individuals who do become symptomatic, viral loads are the highest in the presymptomatic and early symptomatic phase, decreasing thereafter6 7 8 9 10 11 12.
-
Respiratory droplets from infected individuals are a major mode of transmission13. This understanding is the basis of the recommendations for physical distancing, and of the PPE guidance for healthcare workers14. Droplets do not only come from coughing or sneezing: in a-/pre-symptomatic individuals, droplets are generated via talking and breathing15.
-
Face masks reduce droplet dispersal. Cloth-based face masks reduce emission of particles by variable amounts, for example Anfinrud et al15 showed that they are almost completely eliminated. Davies et al16 showed that cloth masks filtered viral particles during coughing at about 50 to 100% of the filtration efficiency of surgical masks, depending on fabric, with absolute filtration efficiencies of 50-70%, and about 70-80% for oral bacteria. van der Sande et al17 showed 50% filtering efficiency for airborne particles.
This evidence supports the conclusion that more widespread risk-based face mask adoption can help to control the Covid-19 epidemic by reducing the shedding of droplets into the environment from asymptomatic individuals. This is also consistent with the experiences of countries that have adopted this strategy.
Our analysis focuses on the effect of face masks on onward virus transmission, or source control18, of infected but symptom-free wearers. This is to be distinguished from the use of face masks as personal protection against virus acquisition. We have found only two randomised control trials in the primary literature on the use of face masks to reduce onward transmission; one19 was underpowered, and the other20 showed significant reduction when adjusted for actual mask usage in a posthoc analysis. One non-randomized study showed that mask use to prevent onward transmission significantly reduced viral respiratory tract infection in immunocompromised patients.21 Greenhalgh et al22 and Javid et al23 argue that “absence of evidence” should not be misinterpreted as “evidence of absence”, and in support of face mask usage by the public based on the precautionary principle.
Policy implications
-
Strategies to transition out of lockdown need to take into account the role of both symptomatic and asymptomatic individuals in spreading Covid-19. Face masks can reduce viral shedding into the environment from such individuals. Both commercially available and homemade cloth masks and surgical masks can play a role.
-
Face masks may play an important role in situations where social distancing is not possible or unpredictable. These situations include public transport, stores and shopping areas, work places, within households, clinics, hospitals, care-homes, social care, and busy pavements. If used widely and correctly and on a risk basis, face masks, including homemade cloth masks, can reduce viral transmission: benefits of use increase where risk exposure is high and are marginal where its low.
-
Public health interventions that involve cost to the public and access to reliable information tend to be taken up faster, more widely or more effectively by higher socio-economic status groups. If the use of cloth face masks in public is made mandatory or highly recommended, interventions may be necessary to ensure that all members of the public have access to these masks and information about proper use, including guidance on washing and re-use appropriate to the domestic environment to ensure that masks themselves do not become fomites..
-
While there is anecdotal evidence of individual risk compensation behaviour, at a population level the introduction of safety measures like HIV prevention measures, seatbelts and helmets have led to increased safety and even increased safety oriented behaviour24. There is no evidence for individual risk compensation amongst the public during epidemics.
-
Clear instructions, that they should be worn in addition to other government measures like physical distancing and handwashing, and that they primarily protect others rather than the wearer, will be necessary to support correct use and avoid risk compensation behaviour. The establishment of standards for manufactured and homemade cloth face masks, as has been done for other areas of public health, is one approach to achieving this.
-
In parallel with any policy recommending the use of cloth face masks for the general public, it will be necessary to take all steps to ensure sufficient supply of surgical masks as well as PPE for frontline NHS and social care workers. Use of cloth face masks by the public must not compete with or compromise the supply of PPE for clinical use.
This summary represents the main conclusion of the DELVE Initiative on the wearing of face masks in public, based on a review of the primary literature, and new data-enabled analyses. This evidence base supports the conclusion that appropriate use of surgical and cloth, including homemade, face masks among the public can have a mitigating effect on the spread of Covid-19.
Technical annexes to this document provide detailed analyses, review additional considerations, and highlight particular practical issues of importance.
Areas where further investigation is needed
-
While there is good indirect supporting evidence that suggests droplets are a main transmission route, the relative contribution of droplet transmission has not yet been directly established empirically.
-
Evidence on the extent of transmission from those who remain asymptomatic as opposed to pre-symptomatic transmissions is evolving. Further work on population testing and transmission studies is needed to address these gaps.
-
Since risk exposure varies (from 0 to 1), it follows that advice on mask wearing is most useful if it is risk based. Further work is recommended to evaluate & categorise risk exposure, in order to give the public practical advice on when mask use is most and least necessary. Until such studies are definitive, it may be useful to consider whether simple common-sense guidelines could be a constructive interim measure where it is likely that physical distancing may be difficult or unpredictable.
-
Mask efficacy depends on material, fit, and other factors. It follows that guidance on risk exposure would be useful (when is a cloth mask adequate, what activity would merit a well-fitted higher-grade mask?).
Evidence Base
Current understanding of transmission mechanism and public mask wearing
What proportion of transmissions are asymptomatic/presymptomatic?
There is evidence of transmissions from both infected asymptomatic individuals, as well as from presymptomatic individuals, i.e., infectious individuals who will go on to display symptoms but are asymptomatic at the time of transmission25 26. Mechanistically, this is related to the high viral load typical of SARS-CoV-2 at the time of symptom onset, as well as evidence of viral shedding occurring prior to the appearance of symptoms27 28. One recent paper estimated contributions to the overall reproduction number $R_0$ arising from asymptomatic ($R_a$), presymptomatic ($R_p$), symptomatic ($R_s$), and environmental transmission ($R_e$), i.e. $R_0=R_a+R_p+R_s+R_e$, and found ratios of $R_a$:$R_p$:$R_s$:$R_e$ = 1:9:8:22. Note that in this paper, environmental transmission is defined as transmission via contamination; in other words in a way that would not be attributable to contact with the infected source2. This is broadly consistent with estimates of 46%-55% presymptomatic transmission in He et al29 as well as estimates of 48% and 62% in data from Singapore and Tianjin30. We note that one report estimated that prior to the implementation of travel restrictions on January 23, 2020, in China, up to 79% of documented cases arose from undocumented infections, many of whom were likely not severely symptomatic31.
What proportion of transmissions are from droplets vs aerosols?
It is currently believed that droplets are the main route of transmission. Whilst there is indirect evidence that supports this, the relative contribution of droplet/aerosol transmission has not been estimated.
Aerosols refer to suspensions in gas of small particles (typically < 5-10 µm) and can travel relatively long distances. Droplets refer to large particles (> 20 µm) and can only travel short distances as they will fall to ground due to gravity32. While the possibility of aerosol transmission of COVID-19 has been clearly demonstrated through experiments33 and outbreak reports (e.g., Washington state choir34), it remains unclear what proportion of infection can be attributed to aerosol transmission. Some studies provide indirect evidence that droplets may be the main routes of transmission. For example, a recent report by Lu et al35 describes an outbreak in a restaurant in Guanzhou, China, in which customers were likely to have been infected through droplets that travelled through air conditioning airflow; they conclude that the patterns of outbreak is consistent with droplet transmission, rather than aerosol transmission. Anfinrud et al15 demonstrates that droplets, smaller than those generated through coughing or sneezing, can be generated via speech, providing further evidence that droplet transmission may play important roles. Public Health England36 also suggests that droplets and contacts are main routes of transmission. It is currently unknown what proportion of infected cases can be attributed to aerosol vs droplet transmission.
What proportion of transmissions occur indoors vs outdoors?
Recent analysis from China suggests that a large proportion of transmission occurs indoors, particularly within homes and on transport.
Many outbreak reports describe indoor transmission, including transmission within homes, churches37, hospitals38, gyms, and restaurants39. However, there may be selection bias as indoor transmission is easier to trace and identify. Qian et al40 analyzed 318 outbreaks, involving 3 or more cases, between January 4 and February 11, from China, outside of Hubei province, and found that 80% of the outbreaks are home outbreaks and 34% are transport outbreaks (some outbreaks belong to more than one category); they identified one outbreak in the outdoor setting.
What are the effects of cloth or homemade masks relative to surgical masks on droplet/aerosol spread and on viral load?
In addition to events such as coughs and sneezes producing respiratory emissions, speech has also been found to produce substantial numbers of droplets capable of containing respiratory pathogens15. To this effect, several studies have assessed the usefulness of different types of masks in mitigating emissions from an individual to the environment. Masks made from cloth or household materials have been found to filter pathogens less effectively than surgical masks, with efficiency estimates relative to surgical masks ranging from approximately 70% in a study using bacteria and bacteriophage41, to approximately 50% in a study of airborne particles42.
In terms of viral load, in a study of influenza, viral RNA was detected in coarse (greater than 5 micron) particles from 11% of the volunteers when they wore surgical masks, and from 43% of the volunteers when they did not. In fine particles (less than 5 micron in size), viral RNA was detected from 78% of individuals when wearing surgical masks and from 92% of individuals when they did not43. This study concluded that the surgical masks produced a 3.4 fold (95% CI 1.8 to 6.3) reduction in viral copies in exhaled breath. Another recent study found that for coronaviruses, surgical face masks reduced virus shedding in respiratory droplets (greater than 5 micron) and aerosols (less than 5 micron) emitted by symptomatic individuals44. Specifically, coronaviruses were detected in 30% and 40% of droplet and aerosol samples, respectively, from symptomatic individuals not wearing masks, and in no samples for both droplets and aerosols for symptomatic individuals wearing surgical masks45.
Can masks be decontaminated and re-used?
A few studies (e.g., Mills et al 201846 and Lore et al 201247) have demonstrated that N95 masks can be reused if properly decontaminated (e.g., by using Ultraviolet irradiation). There are multiple studies on the effect of different decontamination procedures, and that these will need to be considered in the development of any guidance on mask use. A recent study by Kumar et al48 showed that decontamination of SARS-CoV-2 on N95 masks can be done without impairing their filtration efficiency for up to 10 cycles depending on the decontamination method. Optimal decontamination procedures for cloth masks need to be determined urgently.
Observational and RCT Studies of Community Mask Wearing
Is there direct evidence on mask wearing in the community for decreasing onward transmission?
Virtually all studies on mask usage are focused on their use for the protection of the wearer. These include the studies that are the subject of current meta-analyses and reviews49 50 51. Such studies do not answer the question of whether mask use will provide source control.
To our knowledge, only two studies have been performed that studied the effectiveness of mask use by the source patient with a viral respiratory infection (mostly influenza) and tracking the development of viral infection symptoms in others. Both studies used surgical masks and monitored transmission to household members. Both studies have flaws, the most serious of which were sample sizes that were too low or an unexpectedly mild respiratory virus season. One additional study examined the rates of viral respiratory tract infection in bone marrow transplant patients when all health care workers and visitors to the hospital ward wore surgical masks in comparison to infection rates prior to the masking period.21
The study by Canini et al52 was stopped early because of poor enrollment; the study had only a 38% chance of detecting a 40% additional protection by masking. Not unexpectedly, the study found no masking effectiveness.
McIntyre et al53 studied the effectiveness of the use of a surgical mask placed on a subject with a viral respiratory infection living in a household of two or more people. They found that 15% of subjects not assigned to mask wearing wore them, while 2% of subjects assigned to wear them did not. Also, probably owing to a mild flu season, only 1 to 2% of household contacts developed illness versus the expected 20%. This resulted in only a 9% chance of detecting a 50% decrease in illnesses in mask-wearing households. However, after adjustments for mask wearing in the index cases, the study found that wearing a surgical mask by the infected person reduced the frequency of viral respiratory infection in household members by 77% (95% CI 11 to 94% reduction).
It is important to note in both studies that mask wearing by the source subjects was still infrequent, around 4 hours a day in both studies. Because of the infrequent use of masks by the source patients, any effect measured can be considered a minimal estimate when considering a recommendation that masks be worn 100% of the time when physical distancing is not possible or predictable in public. These studies focused on the use of surgical masks, rather than cloth, limiting extrapolation.
Sung et al21 studied the effect of a change in surgical mask use on a bone marrow transplant use over a four-year period. Prior to this change, masks were not worn routinely on the unit. Because the patients were hospitalized for longer than the incubation period of viral respiratory tract infections, and were in a HEPA-filtered protective environment, all viral respiratory tract infections in the patients were due to transmission from health care workers and visitors. In comparison to the frequency of viral infection prior to universal mask use, mask use resulted in about a 2.5-fold decrease in patient infections for laboratory-confirmed viral infections, the majority of which were parainfluenza viral infections (p<0.001). To adjust for seasonal and yearly variations in respiratory virus infections, a time-series analysis was conducted, showing a significant reduction (60%, p = 0.02) in viral infections due to mask use. Mask compliance was very high, >98%, for both healthcare workers and visitors. A limitation of this study is its before-after design.
Behavioural considerations
Does wearing masks lead to more risky behaviour?
There is anecdotal evidence that masks can encourage negative behaviours in professional settings (for instance industry). This is attributable to desensitisation from extended wear and familiarity with the hazardous material. However, there is no direct evidence that this is the case in public settings where there is less chance for desensitisation. Further, at a population level past introductions of safety measures like HIV prevention measures, seatbelts and helmets have led to increased safety and even increased safety oriented behaviour54.
Will universal use of face masks be accepted by the public?
Survey data shows a high uptake of different forms of masks in Italy (81%), a country with no history of widespread mask wearing55. An April 15th survey of 1,500 Britons found that 41% of respondents believed that the public should be asked to wear masks, compared to 33% who disagreed56 so there is some public support for this.
Insights from behavioural science suggest:
-
Because people view an action as correct in a given situation to the degree that they see others performing it57 58, there is an advantage to encouraging universal application in appropriate settings (such as public transport), with the aim of developing a critical mass of adherence and setting new norms around mask use.
-
Because such norms act to inform observers that normative behaviour is both pragmatically prudent and morally proper59, information campaigns should convey that others are undertaking proper conduct for both practical and moral reasons, as that combination produces the greatest adherence60 61.
-
Because, especially in the case of new norms, adherence to a specific form of normative conduct can spur adherence to related forms of normative conduct62, the visibility of masks can be expected to act as a reminder of the need for physical distance, increased hand washing, reduced face touching, and group solidarity.
-
Because newly installed norms are unfamiliar and potentially unclear, explicit instructions about mask use (e.g., how to wear for adequate coverage and when to end mask use) may be necessary.
International responses
What do we know about policy and impact of mask wearing in other countries?
The general approach among countries with policies in place for mask use is to encourage a variety of materials to be used for face masks. Countries that have implemented widespread use of masks early in their national outbreak tend to have flatter curves than those that do not and several officials cite implementing mask policies due to asymptomatic transmission as a reason for this. Whilst this evidence is consistent with a beneficial mask effect, many other factors complicate this picture. Prior experience has been suggested as a factor influencing the nature and implementation of public health policy in countries with outbreaks of SARS and MERS.63
-
Policies and Mask Types
In Europe, policy recommendations are mostly geared towards encouraging use of homemade or other non-surgical facial masks for the general population with the aim of providing readily-available protection, while reducing the risks of a limited surgical mask supply becoming unavailable for the healthcare professionals. Mask policies range from recommendations of different forms of homemade masks, from cloths, scarves and bandanas in Germany and the Czech Republic - with fines administered for non-compliance - to government-controlled surgical mask distribution in local pharmacies, such as KF94 masks in South Korea and N95 masks in Taiwan64. More information on country policies are attached in the Appendix.
-
Impact
The difference in the rate of increase in cases after the 100th confirmed case in European countries with little or no mask wearing practices such as Spain and Italy, and Asian countries such as Taiwan and Hong Kong with stringent mask policies is notable (see figure below). However, it should be noted that New Zealand’s approach - which relies heavily on aggressive testing, tracing and quarantining of virus carriers, with lockdown measures in place - does not include universal mask policies65.
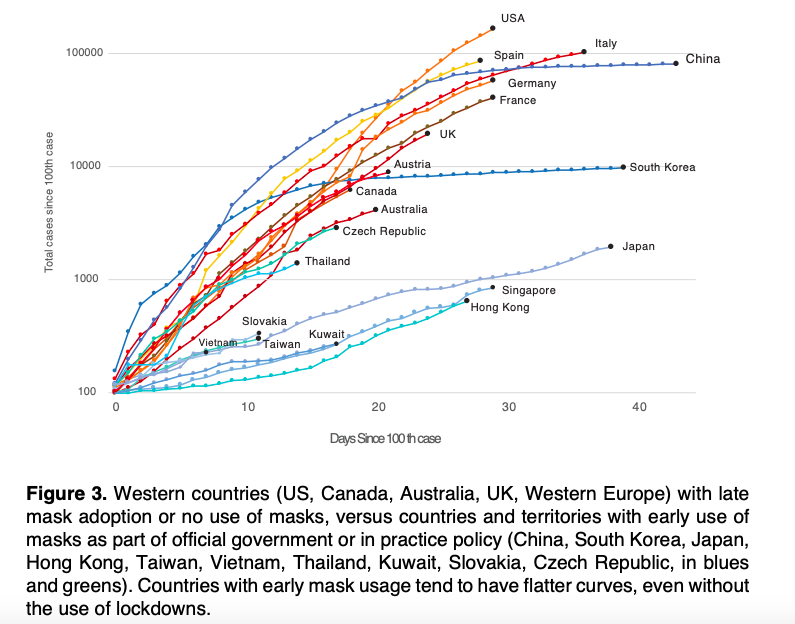
Fig. 1: Retrieved from Longrich and Sheppard (2020)66.
Korea’s government has also witnessed an uptake in mask use due to ease of access: the number of pharmacies that sold all of their mask supplies increased from 67.9% to 86.4% in 11 days67.
Similarly, in Hong Kong, a recent survey found that “85% of respondents reported avoiding crowded places and 99% reported wearing face masks when leaving home”68. Microbiologist Yuen Kwok-yung from Hong Kong, who helped confirm the spread of COVID-19 in humans has stated that apart from population control, mask-wearing, hand-washing, and social distancing are all necessary and must be implemented early to suppress transmission69. This is indicative that clear guidance on mask use aids mask uptake in the community.
Reasons for implementing public mask policies:
In Singapore, National Development Minister Lawrence Wong cited recent fears of asymptomatic spread as one reason for the country’s introduction of mask wearing: “We updated our advice on masks based on the latest scientific evidence: the finding that people without symptoms or very mild symptoms could be spreading the virus”70.
The Director General of the Chinese Center for Disease Control and Prevention (CDC) highlights the prevention of virus transmission via droplets expelled during speaking in close contact, particularly from asymptomatic and presymptomatic carriers, in their guidance: “The big mistake in the U.S. and Europe, in my opinion, is that people aren’t wearing masks. Many people have asymptomatic or presymptomatic infections. If they are wearing face masks, it can prevent droplets that carry the virus from escaping and infecting others”71.
In Germany, the Robert Koch Institute, the national disease control and prevention agency stated that “some infected people do not become ill at all (asymptomatic infection), but could still pass it on to others. Therefore, the wearing of temporary masks by people entering public places where the safety distance cannot be maintained, e.g. public transport, grocery stores or even at the workplace, could help to reduce the spread of SARS-CoV-2”72.
WHO recommendations
The current World Health Organization (WHO)’s recommendation is to wear a surgical mask to prevent onward transmission only if the wearer is symptomatic or is treating someone suspected to have been infected by COVID73. However, this inevitably leads to discrepancies arising from transmissions from those exhibiting no symptoms or are in the pre-symptomatic phase74. Further to this, previous studies conducted on the effect of hand hygiene, facemask use and influenza transmission found that hand hygiene alone was insufficient, but when coupled with facemask use, there was reduced transmission75. WHO are carrying out further research to understand the efficacy of non-surgical masks and will update their guidance when new evidence is available76.
Is there evidence that early adoption of public mask wearing in Czech Republic as compared to Austria mitigated epidemic spread?
There is anecdotal77 but no conclusive evidence. Government policies of these neighbouring countries largely overlap, with lockdown occurring on the same day. From lockdown, their relative growths in cumulative infection counts match for 2½ weeks, when Austria follows the Czech Republic and also introduces public mask-wearing. At that point new Austrian cases slow down compared to the Czech Republic.
It is plausible that Austria’s comparative slow-down 2½ weeks after lockdown should instead be attributed to more comprehensive testing, which started 1½ weeks after lockdown. Austria broadened their testing criteria one week before enforcing mask-wearing, testing anyone who shows COVID-19 symptoms, as opposed to only those who also fill narrower criteria (e.g. key workers only). The Czech Republic didn’t broaden their testing criteria like Austria did in that period.
Appendix: Mask policies in different countries
| Country | At what point in the spread of disease were masks introduced? | What form of mask is used? | Who is required to wear a mask? In what circumstances? | How is this enforced? |
| Germany | 31st March 2020: Mask use introduced in city of Jena, 2 weeks after school closures and ban of public gatherings. 15th April 2020: Announcement from Chancellor Merkel that mask-wearing should extend nationwide, following concern of spread via potential asymptomatic carriers. Germany’s first reported case was on 27th January and it is beginning to relax current lockdown measures. |
General public encouraged to use home-sewn masks or wear protective cloth, rather than medical masks, to prevent shortage of supply for medical professionals and essential workers. | For those going outside into public spaces i.e. shoppers, those using public transport. | Certain cities such as Jena have made mask use mandatory, whereas nation-wide these measures are rather recommended. |
| Czech Republic | 19th March 2020: 18 days after the first confirmed case. This occurred at the same time commuting became restricted to essential grocery shopping. | If surgical masks are unavailable for public use, any form of cotton material such as folded bandanas and scarves. | Anyone moving outside their home for any reason. People are required to wear protective medical masks and keep a distance of 2m everywhere. | Initially encouraged through a social media campaign that promoted mask use. Now compulsory by law.. Fines for non-compliance. |
| South Korea | Mid-January 2020: Mask use, particularly for healthcare professionals and those showing respiratory symptoms already in place due to societal practices. 9th March 2020: Mask distribution policy introduced. This is a 5-day rotation system that restricts the number of masks someone can buy, to ensure more equitable distribution and to minimise price-hiking from panic buying. Government bought masks from manufacturers to then distribute to the public to control supply. South Korea’s first reported case was announced on 20th January and infection control seems to be stable. |
General population advised to wear KF80 (i.e. FFP1)-type masks. Those required to wear more protective masks (i.e. KF94): 1. Those showing respiratory symptoms (coughing, sneezing, runny/blocked nose, sore throat, producing sputum). 2. Those taking care of COVID-19 patients. 3. People who visit hospitals or clinics. 4. Those working in areas which require them to contact many people (e.g. bus drivers, salesperson, postman, janitor etc.). |
Everyone in public, especially showing respiratory symptoms. Those in their personal space (e.g. indoors) and non-crowded areas do not need to wear masks. | Regulated and monitored via social security number. Members of the public can go to a pharmacy on an assigned day of the week, allocated by birth year, and can buy only 2 masks per week. ID required to track purchases to prevent multiple purchases from different pharmacies. Mask availability for every pharmacy can be found via a mobile app. |
| China | December 2019: Mask use, particularly for healthcare professionals and those showing respiratory symptoms already in place due to societal practices. 26th January 2020: China’s State Council approved subsidies worth USD $1.63bn for COVID19 efforts to procure more masks. By 27th January, there were nearly 4,500 confirmed cases and 106 deaths The first reported case was in December 2019, whilst the lockdown in Wuhan occurred on 23rd January 2020. 19th March 2020: national guidelines introduced for the general population. |
Surgical or disposable masks for those at moderate risk of infection: 1. Those working in crowded areas (e.g. hospitals, train stations). 2. Those in contact with someone in quarantine. 3. Those likely to come into contact with COVID19-infected people (e.g. police). Low-risk people should wear disposable masks e.g. those visiting hospitals. A mask should not be used for more than 8 hours in total. |
Those in public areas likely come across other members of the public. | Some provincial differences in enforcement/penalties but it is generally mandatory. |
| U.S.A.: State of New York | 15th April 2020: Governor Cuomo of New York in the process of issuing an executive order to make face coverings obligatory for residents, to take effect on 17th April. The state’s first confirmed case was reported on 1st March; schools and non-business were closed as restrictive measures were put in place from 15th March. New York, New Jersey and Maryland are so far the only states to have issued broad orders mandating face coverings in most public settings in the US. | Any form of face covering that masks the mouth and nose; examples include protective masks, scarves and bandanas | Anyone not able to maintain social distancing measures in public and/or crowded areas e.g. on public transport, sidewalks and shops. This is in line with non-binding guidelines from the Centers for Disease Control and Prevention | Cuomo stated that these rules enforced by local governments but no one would be forcibly removed from public transport for non-compliance. Consideration of issuing civil, not criminal, penalties. |
Additional Material
The following is a list of additional material associated with this report from the DELVE initiative.
- MAS-TD1: Report on Face Masks for the General Public - An Update
Prepared for the DELVE Initiative by
Footnotes and References
-
He X et al. 2020 Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med (doi: 10.1038/s41591-020-0869-5). ↩
-
Ferretti L et al. 2020 Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science (doi: 10.1126/science.abb6936). ↩ ↩2 ↩3
-
Ganyani, T et al. 2020 Estimating the generation interval for COVID-19 based on symptom onset data. medRxiv (doi: 10.1101/2020.03.05.20031815). ↩
-
Li R et al. 2020 Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2). Science (doi: 10.1126/science.abb3221). ↩
-
Sutton D, Fuchs K, D’Alton M, Goffman D. 2020 Universal screening for SARS-COV2 in women admitted for delivery. NEJM (doi: 10.1056/NEJMc2009316). ↩
-
Pan X et al. 2020 Asymptomatic cases in a family cluster with SARS-CoV-2 infection. The Lancet Infectious Diseases (doi: 10.1016/S1473-3099(20)30114-6). ↩
-
Zou L et al. 2020. SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients. NEJM (doi:10.1056/NEJMc2001737). ↩
-
Bai Y et al. 2020 Presumed Asymptomatic Carrier Transmission of COVID-19. JAMA (doi: 10.1001/jama.2020.2565). ↩
-
Hodcroft EB. 2020 Preliminary case report on the SARS-CoV-2 cluster in the UK, France, and Spain. Swiss Medical Weekly (doi:10.4414/smw.2020.20212). ↩
-
He X et al. 2020 Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med (doi: 10.1038/s41591-020-0869-5). ↩
-
Tan W et al. 2020 Viral Kinetics and Antibody Responses in Patients with COVID-19. MedRxiV (doi: 10.1101/2020.03.24.20042382). ↩
-
Wölfel, R. et al. (2020). Virological assessment of hospitalized patients with COVID-2019. Nature (doi: 10.1038/s41586-020-2196-x). ↩
-
World Health Organization. 2020 Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. See https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations. ↩
-
Public Health England. 2020 COVID-19: infection prevention and control guidance, see https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/881489/COVID-19_Infection_prevention_and_control_guidance_complete.pdf ↩
-
Anfinrud P, Stadnytskyi V, Bax CE, Bax A. 2020 Visualizing Speech-Generated Oral Fluid Droplets with Laser Light Scattering. New England Journal of Medicine (doi: 10.1056/NEJMc2007800). ↩ ↩2 ↩3 ↩4
-
Davies A et al. 2013 Testing the efficacy of homemade masks: would they protect in an influenza pandemic?. Disaster Medicine and Public Health Preparedness (doi: 10.1017/dmp.2013.43). ↩
-
van der Sande M, Teunis P, Sabel, R. 2008 Professional and home-made face masks reduce exposure to respiratory infections among the general population. PLoS One (doi: 10.1371/journal.pone.0002618). ↩
-
Howard J. 2020. To help stop coronavirus, everyone should be wearing face masks. The science is clear. The Guardian. See https://www.theguardian.com/commentisfree/2020/apr/04/why-wear-a-mask-may-be-our-best-weapon-to-stop-coronavirus ↩
-
Canini L et al 2010. Surgical mask to prevent influenza transmission in households: A cluster randomized trial. PLoS One (doi: 10.1371/journal.pone.0013998). ↩
-
MacIntyre C, Zhang Y, Chughtai A, et al. 2016. Cluster randomised controlled trial to examine medical mask use as source control for people with respiratory illness. BMJ Open (doi: 10.1136/bmjopen-2016-012330 ↩
-
Sung AD, Sung JAM, Thomas S, et al. 2016. Universal Mask Usage for Reduction of Respiratory Viral Infections After Stem Cell Transplant: A Prospective Trial. Clin Infect Dis, 63, 999-1006 (doi: 10.1093/cid/ciw451). ↩ ↩2 ↩3
-
Greenhalgh T et al. 2020. Face masks for the public during the covid-19 crisis. BMJ (doi: 10.1136/bmj.m1435). ↩
-
Javid B, Weekes MP, Matheson NJ. 2020 Covid-19: should the public wear face masks? BMJ (doi: 10.1136/bmj.m1442). ↩
-
Howard J. 2020. To help stop coronavirus, everyone should be wearing face masks. The science is clear. The Guardian. See https://www.theguardian.com/commentisfree/2020/apr/04/why-wear-a-mask-may-be-our-best-weapon-to-stop-coronavirus ↩
-
Rothe C et al. 2020 Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. NEJM (doi: 10.1056/NEJMc2001468). ↩
-
Kimball A et al. 2020 Asymptomatic and Presymptomatic SARS-CoV-2 Infections in Residents of a Long-Term Care Skilled Nursing Facility — King County, Washington, March 2020. MMWR Morbidity and Mortality Weekly Report. See https://www.cdc.gov/mmwr/volumes/69/wr/mm6913e1.htm ↩
-
He X et al. 2020 Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med (doi: 10.1038/s41591-020-0869-5). ↩
-
Zou L et al. 2020. SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients. NEJM (doi: 10.1056/NEJMc2001737). ↩
-
He X et al. 2020 Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med (doi: 10.1038/s41591-020-0869-5). ↩
-
Ganyani, T et al. 2020 Estimating the generation interval for COVID-19 based on symptom onset data. medRxiv (doi: 10.1101/2020.03.05.20031815). ↩
-
Li R et al. 2020 Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2). Science (doi: 10.1126/science.abb3221). ↩
-
Tellier R, Li Y, Cowling BJ, Tang JW. 2019 Recognition of aerosol transmission of infectious agents: a commentary. BMC Infectious Diseases (doi: 10.1186/s12879-019-3707-y). ↩
-
van Doremalen N et al. 2020 Aerosol and Surface Stability of HCoV-19 (SARS-CoV-2) Compared to SARS-CoV-1. MedRxiv (doi: 10.1056/NEJMc2004973). ↩
-
Los Angeles Times. 2020 A choir decided to go ahead with rehearsal. Now dozens of members have COVID-19 and two are dead. See https://www.latimes.com/world-nation/story/2020-03-29/coronavirus-choir-outbreak. ↩
-
Lu P et al. 2020. COVID-19 Outbreak Associated with Air Conditioning in Restaurant, Guangzhou, China. Emerging Infectious Diseases (doi: 10.3201/eid2607.200764). ↩
-
Public Health England. 2020 Transmission characteristics and principles of infection prevention and control. See https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/transmission-characteristics-and-principles-of-infection-prevention-and-control ↩
-
Wei WE et al. 2020 Presymptomatic Transmission of SARS-CoV-2 — Singapore, January 23–March 16, 2020. MMWR Morbidity and Mortality Weekly Report. See https://www.cdc.gov/mmwr/volumes/69/wr/mm6914e1.htm?fbclid=IwAR1b_S3wC7pqWsIF5wUhjMqQWXbxA6rc-YLy80so8Vcxx7160WQHHB0wxm4 ↩
-
Bai Y et al. 2020 Presumed Asymptomatic Carrier Transmission of COVID-19. JAMA (doi: 10.1001/jama.2020.2565). ↩
-
Lu P et al. 2020. COVID-19 Outbreak Associated with Air Conditioning in Restaurant, Guangzhou, China. Emerging Infectious Diseases (doi: 10.3201/eid2607.200764). ↩
-
Qian H et al. 2020 Indoor transmission of SARS-CoV-2. MedRxiv (doi: 10.1101/2020.04.04.20053058). ↩
-
Davies A et al. 2013 Testing the efficacy of homemade masks: would they protect in an influenza pandemic?. Disaster Medicine and Public Health Preparedness (doi: 10.1017/dmp.2013.43). ↩
-
van der Sande M, Teunis P, Sabel, R. 2008 Professional and home-made face masks reduce exposure to respiratory infections among the general population. PLoS One (doi: 10.1371/journal.pone.0002618). ↩
-
Milton DK et al. 2013 Influenza Virus Aerosols in Human Exhaled Breath: Particle Size, Culturability, and Effect of Surgical Masks. Plos Pathogens (doi: 10.1371/journal.ppat.1003205). ↩
-
Leung NHL et al. 2020 Respiratory virus shedding in exhaled breath and efficacy of face masks. Nature Medicine (doi: 10.5061/dryad.w9ghx3fkt). ↩
-
Leung NHL et al. 2020 Respiratory virus shedding in exhaled breath and efficacy of face masks. Nature Medicine (doi: 10.5061/dryad.w9ghx3fkt). ↩
-
Mills D et al. 2018 Ultraviolet germicidal irradiation of influenza-contaminated N95 filtering facepiece respirators. American Journal of Infection Control (doi: 10.1016/j.ajic.2018.02.018). ↩
-
Lore M et al. 2012 Effectiveness of Three Decontamination Treatments against Influenza Virus Applied to Filtering Facepiece Respirators, The Annals of Occupational Hygiene (doi: 10.1093/annhyg/mer054). ↩
-
Kumar et al. 2020 N95 Mask Decontamination using Standard Hospital Sterilization Technologies. MedRxiv (doi: 10.1101/2020.04.05.20049346). ↩
-
Brainard JS et al. 2020 Facemasks and similar barriers to prevent respiratory illness such as COVID-19: A rapid systematic review. MedRxiv (doi: 10.1101/2020.04.01.20049528). ↩
-
Xiao J, Shiu EYC, Gao H, et al. 2020. Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings-Personal Protective and Environmental Measures. Emerg Infect Dis, 26, 967-75. https://www.ncbi.nlm.nih.gov/pubmed/3202758610.3201/eid2605.190994. ↩
-
Cowling BJ, Zhou Y, Ip DK, Leung GM, Aiello AE. 2010. Face masks to prevent transmission of influenza virus: a systematic review. Epidemiol Infect, 138, 449-56. https://www.ncbi.nlm.nih.gov/pubmed/2009266810.1017/S0950268809991658. ↩
-
Canini L et al 2010. Surgical mask to prevent influenza transmission in households: A cluster randomized trial. PLoS One (doi:10.1371/journal.pone.0013998). ↩
-
MacIntyre CR et al. 2009 Face mask use and control of respiratory virus transmission in households. Emerg Infect Dis (doi:10.3201/eid1502.081166). ↩
-
Howard J. 2020. To help stop coronavirus, everyone should be wearing face masks. The science is clear. The Guardian. See https://www.theguardian.com/commentisfree/2020/apr/04/why-wear-a-mask-may-be-our-best-weapon-to-stop-coronavirus ↩
-
Ipsos MORI. 2020 More people say they’re wearing masks to protect themselves from COVID-19 since March. See https://www.ipsos.com/en/more-people-say-theyre-wearing-masks-protect-themselves-covid-19-march ↩
-
The Telegraph. 2020 Support for wearing face masks in public outweighs opposition, 18 April. See https://www.telegraph.co.uk/news/2020/04/18/public-support-wearing-face-masks-public-outweighs-opposition/ ↩
-
Farrow K, Grolleau G, Ibanez L. 2017. Social norms and pro-environmental behavior: A review of the evidence. Ecological Economics (doi: 10.1016/j.ecolecon.2017.04.017). ↩
-
Frank RH. 2020 Under the Influence: Putting peer pressure to work. Princeton University Press (ISBN: 9780691193083). ↩
-
Nolan JM, Schultz PW, Cialdini RB, Goldstein NJ. 2020 The Social Norms Approach: A Wise Intervention for Solving Social and Environmental Problems. Handbook of Wise Interventions. ↩
-
Jacobson RP et al. 2020 The Synergistic Effect of Descriptive and Injunctive Norm Perceptions on Counterproductive Work Behaviors. Journal of Business Ethics (doi:10.1007/s10551-018-3968-1). ↩
-
Cialdini R. 2020 Advice for Reducing Undesirable COVID-19 Behaviors. See https://www.influenceatwork.com/inside-influence-report/advice-for-reducing-undesirable-covid-19-behaviors/ ↩
-
Mortensen CH et al. 2017 Upward trends: A lever for encouraging behaviors performed by the minority. Social Psychology and Personality Science (doi:10.1177%2F1948550617734615). ↩
-
The Guardian 2020. Experience of Sars a key factor in countries’ response to coronavirus. 15 March 2020. See: https://www.theguardian.com/world/2020/mar/15/experience-of-sars-key-factor-in-response-to-coronavirus ↩
-
Wong T. 2020 Coronavirus: Why some countries wear face masks and others don’t. 31 March. BBC News. See https://www.bbc.co.uk/news/world-52015486 ↩
-
Hollingsworth J. 2020 New Zealand reported a decline in new coronavirus cases for the fourth consecutive day. The country is still tightening its border restrictions. 9 April. CNN. See https://edition.cnn.com/2020/04/09/asia/new-zealand-lessons-intl-hnk/index.html ↩
-
Longrich N, Sheppard S. 2020 Public use of face masks to control the coronavirus (SARS-Cov-2) pandemic: a review of theory and evidence. Preprints. 2020040021 See https://www.preprints.org/manuscript/202004.0021/v2/download. ↩
-
Government of Korea. 2020. Flattening the curve on COVID-19: How Korea responded to a pandemic using ICT. See http://www.korea.kr/common/download.do?fileId=190536078&tblKey=GMN ↩
-
Cowling B et al. 2020 Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health (doi: 10.1016/S2468-2667(20)30090-6). ↩
-
Li I, Zuoyan Z. 2020 Q&A with HK microbiologist Yuen Kwok-yung who helped confirm coronavirus’ human spread. 10 March. The Straits Times. See https://www.straitstimes.com/asia/east-asia/exclusive-qa-with-hong-kong-microbiologist-yuen-kwok-yung-who-helped-confirm ↩
-
CNA. 2020. COVID-19: Why Singapore changed its guidance on masks and made it mandatory. 14 April. Youtube. See https://www.youtube.com/watch?v=dWxfZjH2kf8 ↩
-
Cohen, J. 2020. Not wearing masks to protect against coronavirus is a ‘big mistake,’ top Chinese scientist says. 27 March. ScienceMag. See https://www.sciencemag.org/news/2020/03/not-wearing-masks-protect-against-coronavirus-big-mistake-top-chinese-scientist-says ↩
-
The Local. 2020 Germany recommends face masks in shops and public transport. 15 April. See https://www.thelocal.de/20200415/german-government-pushes-to-make-masks-mandatory-in-public-transport-and-retail ↩
-
World Health Organization. 2020 Coronavirus disease (COVID-19) advice for the public: When and how to use masks. See https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks ↩
-
He X et al. 2020 Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med (doi: 10.1038/s41591-020-0869-5). ↩
-
Wong V, Cowling B, Aiello A. 2014 Hand hygiene and risk of influenza virus infections in the community: A systematic review and meta-analysis. Epidemiol Infect (doi:10.1017/S095026881400003X). ↩
-
Devlin H, Campbell D. 2020 WHO considers changing guidance on wearing face masks. 1 April. The Guardian. See https://www.theguardian.com/world/2020/apr/01/all-uk-hospital-staff-and-patients-should-wear-masks-says-doctors-group#maincontent ↩
-
Greenhalgh T and Howard J. 2020 Masks for all? The science says yes. See https://www.fast.ai/2020/04/13/masks-summary/ ↩